Introduction
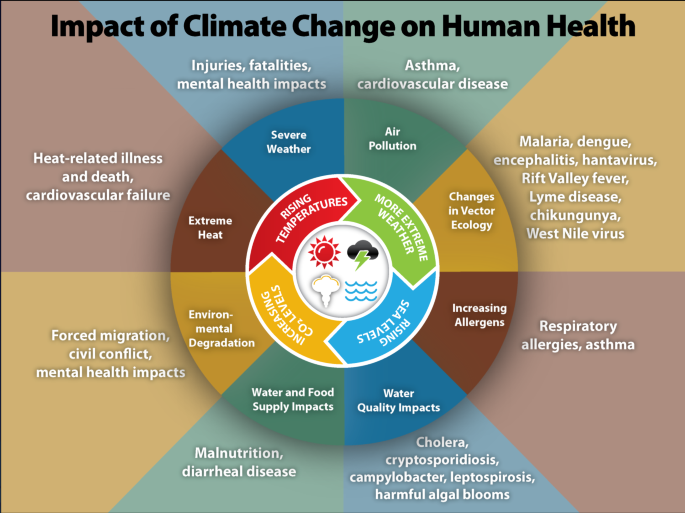
Weather-related illnesses are a growing concern as the world experiences increasingly erratic weather patterns and extreme events due to climate change. These conditions not only pose significant health risks but also have substantial implications for healthcare costs. In this article, we will explore the intersection of healthcare costs and weather-related illnesses, shedding light on the financial burdens faced by individuals, healthcare systems, and governments.
The intersection of healthcare costs and weather-related illnesses is a multifaceted challenge that demands attention and innovative solutions:
Direct Medical Costs: Weather-related illnesses lead to a surge in direct medical costs. Patients require medical treatment for conditions like heatstroke, frostbite, respiratory issues from wildfires, and waterborne diseases following floods. Emergency room visits, hospital stays, medications, and medical procedures contribute to substantial healthcare expenses.
Increased Healthcare Demand: Extreme weather events often lead to a sudden spike in healthcare demand. Hospitals and healthcare facilities must expand their capacity and resources to accommodate the influx of patients. This surge capacity can strain healthcare systems, requiring additional staffing and infrastructure, which comes with a financial burden.
Chronic Health Conditions: Climate change can exacerbate chronic health conditions. For example, individuals with respiratory ailments may experience worsened symptoms due to increased air pollution from wildfires or heat-related exacerbations. The long-term management of these conditions results in ongoing healthcare costs.
Mental Health Impact: Extreme weather events and the resulting displacement, trauma, and loss can have a profound impact on mental health. The treatment and support needed for mental health issues stemming from weather-related disasters contribute to healthcare expenses.
Disaster Preparedness: Healthcare systems and governments invest in disaster preparedness and response measures to ensure timely and effective healthcare delivery during extreme events. These investments include stockpiling medical supplies, training healthcare professionals, and developing response plans, all of which come with financial implications.
Healthcare Infrastructure Resilience: Ensuring the resilience of healthcare infrastructure to withstand extreme weather events is a priority. Hospitals and clinics must be designed and equipped to operate during power outages, flooding, and other adverse conditions. Retrofitting and maintaining resilient healthcare infrastructure require significant investment.
Health Insurance Costs: Weather-related illnesses can lead to higher health insurance premiums. Insurers may pass on the increased costs of covering weather-related health risks to policyholders through higher premiums or deductibles.
Government Healthcare Expenditure: Governments bear a substantial portion of healthcare costs, especially in publicly funded healthcare systems. Weather-related illnesses strain government budgets as they allocate resources to respond to emergencies, support healthcare systems, and provide financial relief to affected individuals.
Healthcare Inequities: Vulnerable populations are disproportionately affected by weather-related illnesses due to socioeconomic disparities. The financial burden on disadvantaged communities is often more significant, exacerbating healthcare inequities.
Public Health Interventions: Public health interventions, such as vaccination campaigns after floods or heat advisories during heatwaves, are crucial for mitigating health risks. These initiatives require funding and coordination.
Addressing the financial impact of weather-related illnesses on healthcare systems and individuals necessitates a multi-pronged approach. This includes investing in climate-resilient healthcare infrastructure, expanding access to healthcare services, improving disaster preparedness, promoting public health education, and implementing policies to reduce greenhouse gas emissions and mitigate climate change. By addressing the intersection of healthcare costs and weather-related illnesses, societies can better protect the health and financial well-being of their populations in a changing climate.
Explore this link for a more extensive examination of the topic: Climate-Related Health Risks Among Workers: Who is at Increased …
As temperatures soar, the risk of heat-related illnesses such as heatstroke and heat exhaustion rises. Elderly individuals and those with pre-existing conditions are particularly vulnerable. We will discuss the healthcare expenses associated with treating these conditions and the strain on emergency services during heatwaves.
As heatwaves become more frequent and severe, healthcare systems must allocate significant resources to address the surge in heat-related illnesses. The costs of medical treatments, hospital admissions, and emergency services add to the financial burden. Additionally, the long-term health impacts of heatwaves, especially on vulnerable populations, require ongoing medical care and support. In this context, we will delve into the escalating healthcare expenses and the need for proactive measures to mitigate the impact of heatwaves on public health and healthcare infrastructure.
To expand your knowledge on this subject, make sure to read on at this location: Extreme Heat | Ready.gov

Increased air pollution, allergens, and extreme weather events like wildfires can exacerbate respiratory conditions such as asthma. The article will delve into the healthcare costs of managing respiratory illnesses exacerbated by changing climate patterns.
Climate change is directly linked to an increase in extreme weather events, leading to more frequent and severe health issues. From heat-related illnesses and vector-borne diseases to respiratory problems aggravated by air pollution, the healthcare sector faces rising costs in treating weather-related illnesses. This article explores the growing financial burden on healthcare systems and patients due to the intersection of climate change and health.
For additional details, consider exploring the related content available here Estimating the Health‐Related Costs of 10 Climate‐Sensitive US …

Changing weather patterns influence the geographic distribution of disease vectors like mosquitoes and ticks. This shift can lead to the spread of diseases such as Lyme disease and West Nile virus, resulting in healthcare expenditures for diagnosis, treatment, and prevention.
extend the following idea: “Climate change also affects air quality, contributing to the prevalence of respiratory diseases such as asthma and allergies. Increased pollen production and longer pollen seasons can exacerbate allergic reactions and strain healthcare resources.”
To expand your knowledge on this subject, make sure to read on at this location: Climate Effects on Health | CDC
Extreme weather events can have a profound impact on mental health, leading to conditions like anxiety, depression, and post-traumatic stress disorder (PTSD). We will explore the financial burdens associated with mental health treatments and support services during and after weather-related disasters.
The intersection of extreme weather events and mental health poses a significant financial burden on individuals, healthcare systems, and communities:
Direct Treatment Costs: Weather-related disasters can trigger or exacerbate mental health conditions, leading to increased demand for mental health services. Individuals affected by events like hurricanes, floods, or wildfires may require therapy, counseling, medication, or hospitalization. These treatments come with direct financial costs.
Emergency Services: During and immediately after extreme weather events, emergency mental health services are often required to provide immediate support to individuals experiencing emotional distress. The deployment of crisis intervention teams and the operation of helplines and crisis centers entail financial expenses.
Post-Disaster Trauma: Weather-related disasters leave lasting psychological trauma for survivors, witnesses, and first responders. Post-traumatic stress disorder (PTSD) and other trauma-related conditions necessitate long-term mental health treatment. These ongoing therapies result in sustained healthcare costs.
Workforce Productivity: The mental health impacts of extreme weather events can lead to decreased workforce productivity. Employees may require time off work for treatment or may experience reduced efficiency due to emotional distress. This can result in economic losses for employers and the broader economy.
Educational Impact: Children and students may experience mental health challenges following extreme weather events. These issues can disrupt their education and require additional support services within schools. Schools and educational institutions must allocate resources for counseling and mental health programs.
Community Support Services: Communities affected by weather-related disasters often need increased access to mental health support services. This includes the availability of support groups, community counseling, and outreach programs, which carry financial costs.
Loss of Life: Tragically, extreme weather events can result in loss of life, further exacerbating the mental health challenges faced by survivors and bereaved families. Grief counseling and support services are crucial but can contribute to the overall financial burden.
Insurance Costs: Mental health treatment expenses can be covered by health insurance, which may lead to increased premiums for policyholders if the frequency of weather-related mental health claims rises. These rising premiums can strain household budgets.
Public Health Response: Government agencies and public health organizations must allocate resources for mental health response and recovery efforts. This includes funding for crisis helplines, mental health training for first responders, and public awareness campaigns.
Preventive Measures: Investing in mental health prevention and resilience-building programs can be cost-effective in the long term. These programs aim to equip individuals and communities with coping strategies and resources to mitigate the impact of extreme weather events on mental health.
Socioeconomic Disparities: Vulnerable populations, including low-income individuals and marginalized communities, may face greater financial challenges in accessing mental health services. Addressing healthcare disparities is essential to ensure equitable access to mental health support.
Long-Term Impacts: Mental health conditions resulting from extreme weather events can have long-lasting effects on individuals’ lives, including their ability to work and maintain stable housing. This can lead to ongoing financial struggles.
To address the financial burden associated with mental health impacts of extreme weather events, a comprehensive approach is needed. This includes increased funding for mental health services, improved disaster preparedness and response strategies, reduced stigma surrounding mental health, and policies that prioritize the well-being of individuals and communities affected by climate-related disasters. By investing in mental health resilience and support, societies can better cope with the mental health challenges posed by a changing climate.
To delve further into this matter, we encourage you to check out the additional resources provided here: Estimating the Health‐Related Costs of 10 Climate‐Sensitive US …

Weather-related illnesses often necessitate emergency medical attention, driving up healthcare costs. We will examine the expenses incurred by individuals and healthcare systems due to emergency room visits during extreme weather events.
Extreme weather events can result in a surge of patients seeking emergency medical care, leading to higher healthcare costs. The expenses incurred include not only the immediate medical treatment but also the longer-term follow-up care and rehabilitation for those affected. Moreover, the strain on emergency rooms and healthcare facilities during these events can disrupt regular medical services and increase healthcare system expenses. Addressing these challenges requires a multi-faceted approach, including better preparedness, improved public health initiatives, and resilient healthcare infrastructure, all of which are essential to manage the escalating healthcare costs associated with extreme weather-related illnesses.
To expand your knowledge on this subject, make sure to read on at this location: Estimating the Health‐Related Costs of 10 Climate‐Sensitive US …

Managing weather-related illnesses requires medications, treatments, and follow-up care. We will discuss the financial aspects of medication costs, doctor visits, and hospitalization for weather-induced health conditions.
Addressing weather-related illnesses often involves various medical interventions, including prescription medications, medical consultations, hospitalizations, and post-treatment follow-up care. The financial implications of these healthcare expenses, both for individuals and healthcare systems, are significant. This article examines the economic aspects of managing weather-induced health conditions, shedding light on the financial challenges faced by patients and the healthcare industry.
Additionally, you can find further information on this topic by visiting this page: The Root Causes of Health Inequity – Communities in Action – NCBI …

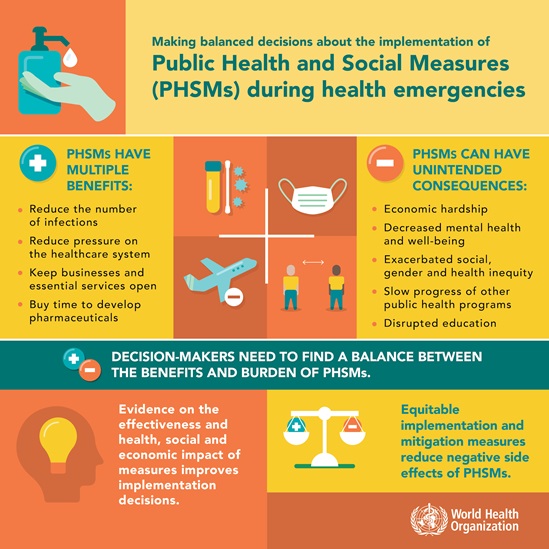
Governments must allocate resources for public health measures, including disaster response and preparedness. We will analyze the budgetary impact of these measures and their role in managing healthcare costs.
In addition to disaster response and preparedness, governments also need to invest in long-term public health strategies. These may include initiatives to promote healthier lifestyles, improve healthcare infrastructure, and enhance disease surveillance. By allocating resources to preventative measures, governments can reduce the overall burden on the healthcare system and control rising healthcare costs over time.
You can also read more about this here: The Health Care Costs of Extreme Heat – Center for American …
Investing in preventive measures and public education on weather-related health risks can reduce the incidence of illnesses and subsequent healthcare costs.
Investing in preventive measures and public education regarding weather-related health risks is a proactive strategy that can yield substantial benefits in terms of reduced illness incidence and healthcare costs:
Early Warning Systems: Implementing robust early warning systems for extreme weather events, such as hurricanes, heatwaves, and wildfires, allows communities to prepare and evacuate if necessary. Timely warnings reduce the likelihood of injuries and illnesses, ultimately reducing healthcare expenses related to disaster response.
Heatwave Preparedness: Public education campaigns can inform vulnerable populations, such as the elderly and those with preexisting health conditions, about the risks of heatwaves and how to stay safe. Encouraging individuals to stay hydrated, stay cool, and seek shelter during heatwaves can prevent heat-related illnesses, reducing hospital admissions and healthcare costs.
Air Quality Alerts: In regions prone to wildfires, public education on air quality alerts is essential. Providing guidance on when it’s safe to be outdoors and when to use masks or air purifiers can help individuals avoid respiratory problems and reduce the need for medical treatment.
Flood Preparedness: Communities in flood-prone areas can benefit from public education on flood preparedness. This includes guidance on safely evacuating flood zones, avoiding contaminated water, and preventing waterborne illnesses. Proactive measures can minimize flood-related health issues and healthcare costs.
Vector-Borne Disease Prevention: In areas susceptible to vector-borne diseases like West Nile virus or Zika virus, public education on mosquito control and protection measures is critical. Using insect repellent, eliminating breeding sites, and raising awareness about disease transmission can reduce the incidence of vector-borne illnesses.
Mental Health Support: Public education campaigns can reduce the stigma around mental health and encourage individuals to seek help when experiencing emotional distress after extreme weather events. Early intervention in mental health issues can prevent more severe conditions and long-term healthcare costs.
Community Resilience: Empowering communities to develop resilience plans and emergency kits can help individuals take proactive steps to protect themselves during extreme weather events. This includes having essential supplies, knowing evacuation routes, and having a communication plan in place.
Disaster Preparedness Kits: Encouraging households to assemble disaster preparedness kits with essential supplies can reduce the strain on healthcare facilities during and after disasters. Having access to clean water, non-perishable food, first aid supplies, and medications can prevent injuries and illnesses.
Local Healthcare Capacity: Public education efforts can inform individuals about the capacity of local healthcare facilities and help them make informed decisions during disasters. Knowing where to seek medical care and understanding healthcare resources available in the community can prevent overcrowding at hospitals.
Climate-Resilient Infrastructure: Investments in climate-resilient infrastructure, such as flood barriers and heat-resistant urban planning, can reduce the impact of extreme weather events on health. These infrastructure improvements protect both individuals’ health and the healthcare system from excessive strain.
Environmental Conservation: Promoting sustainable practices and environmental conservation can mitigate climate change, reducing the frequency and severity of extreme weather events. This, in turn, lowers the overall health risks and healthcare costs associated with such events.
By investing in preventive measures and public education, communities can become more resilient to the health impacts of extreme weather events. These strategies not only reduce the incidence of weather-related illnesses but also alleviate the strain on healthcare systems, ultimately resulting in cost savings and better overall health outcomes for the population.
To delve further into this matter, we encourage you to check out the additional resources provided here: The Root Causes of Health Inequity – Communities in Action – NCBI …
Developing healthcare facilities that can withstand extreme weather events is essential to ensure uninterrupted care and manage costs effectively.
Building healthcare facilities that are resilient to extreme weather events is not only essential for providing uninterrupted care but also for cost-effective healthcare management. Such facilities should be designed and constructed to withstand the physical impact of severe weather, such as hurricanes, floods, and wildfires. They should also incorporate climate-adaptive features to maintain a comfortable and safe environment for patients and healthcare workers during extreme heatwaves or cold snaps. These resilient healthcare facilities not only reduce the risk of damage and disruption but also help manage costs by avoiding expensive repairs, evacuations, and temporary relocations that can occur when facilities are unprepared for extreme weather events. Investing in resilient healthcare infrastructure is a long-term strategy that benefits both patient care and the financial sustainability of the healthcare system.
Looking for more insights? You’ll find them right here in our extended coverage: Building climate-resilient health systems

Policymakers play a crucial role in addressing climate change and its healthcare consequences. We will explore the importance of climate policy in mitigating weather-related health costs.
Policymakers hold a pivotal role in addressing the complex intersection of climate change and healthcare costs. Effective climate policies not only aim to reduce greenhouse gas emissions but also work to mitigate the adverse health effects caused by extreme weather events and changing climate patterns. This article will delve into the significance of climate policies in alleviating the burden of weather-related health costs, emphasizing the need for proactive measures to protect public health and the healthcare system’s financial stability.
To delve further into this matter, we encourage you to check out the additional resources provided here: Climate Effects on Health | CDC

Conclusion
The rising prevalence of weather-related illnesses poses a dual challenge: safeguarding public health and managing escalating healthcare costs. By understanding the financial implications of these illnesses, policymakers, healthcare providers, and individuals can work together to develop strategies for prevention, preparedness, and resilience in the face of climate change.
Indeed, addressing the rising prevalence of weather-related illnesses requires a multi-pronged approach. Here are some key strategies to consider:
Public Health Education: Educating communities about the risks of weather-related illnesses and how to mitigate them is crucial. This can include information on staying hydrated during heatwaves, using insect repellent to prevent vector-borne diseases, and recognizing the signs of weather-related illnesses.
Improved Healthcare Infrastructure: Investing in healthcare infrastructure, particularly in vulnerable regions, can enhance the capacity to diagnose and treat weather-related illnesses promptly. This includes having well-equipped clinics, trained medical professionals, and access to necessary medications.
Disease Surveillance and Early Warning Systems: Developing robust disease surveillance systems that can detect outbreaks early is essential. These systems can help in responding quickly to prevent the spread of illnesses.
Climate-Resilient Communities: Encouraging communities to adopt climate-resilient practices, such as building homes that can withstand extreme weather or creating green spaces to reduce heat island effects, can contribute to preventing weather-related illnesses.
Insurance and Financial Support: Governments and insurance providers can work together to develop insurance products that cover weather-related illnesses. This can help individuals and communities manage the financial burden associated with healthcare costs during extreme weather events.
Climate Mitigation and Adaptation: Finally, addressing the root cause of climate change through mitigation efforts, such as reducing greenhouse gas emissions, is crucial. Simultaneously, adaptation strategies should be in place to deal with the changing climate’s inevitable impacts.
By combining these strategies, communities, healthcare systems, and governments can work together to reduce the prevalence of weather-related illnesses and manage the associated healthcare costs effectively.
For additional details, consider exploring the related content available here Pandemics: Risks, Impacts, and Mitigation – Disease Control …
More links
Additionally, you can find further information on this topic by visiting this page: Climate change and health
