Introduction
Allergic reactions are a common occurrence for many people, ranging from mild skin irritations to severe, life-threatening situations. While most allergic reactions are manageable with over-the-counter antihistamines, some can escalate into anaphylaxis, a severe and potentially fatal condition. Anaphylaxis requires immediate attention and treatment, with epinephrine being a crucial tool in managing this life-threatening allergic reaction. In this article, we will explore the causes and symptoms of anaphylaxis and provide guidance on the proper use of epinephrine to save lives.
Allergic reactions are a pervasive issue affecting individuals of all ages and backgrounds. They can manifest in various forms, from the bothersome itchiness of a mosquito bite to the more serious consequences of ingesting a food allergen. These reactions are essentially the body’s way of responding to substances it perceives as threats, activating the immune system to protect itself.
For most people, allergies are an occasional inconvenience. Over-the-counter antihistamines and topical creams can often provide quick relief, soothing the itch or redness caused by allergens like pollen, pet dander, or certain skincare products. These mild reactions, while uncomfortable, are generally not life-threatening.
However, a subset of allergic responses takes a far more dangerous turn. Anaphylaxis is the extreme end of the spectrum, representing an immediate and severe allergic reaction that can put a person’s life in jeopardy. Anaphylaxis occurs when the body’s immune system goes into overdrive, releasing a flood of chemicals that can lead to a cascade of symptoms affecting various organs and systems.
The symptoms of anaphylaxis are often swift and dramatic. Skin changes such as hives and extreme itching may appear alongside respiratory distress, making breathing difficult. The throat may constrict, leading to a feeling of suffocation, while the heart rate can become dangerously irregular. Nausea, vomiting, and abdominal pain may add to the distress, and in severe cases, individuals can lose consciousness.
It’s crucial to recognize that anaphylaxis demands immediate attention. Without prompt intervention, it can lead to death within minutes. This is where epinephrine, often referred to as adrenaline, becomes the critical tool in managing anaphylactic reactions.
Epinephrine acts swiftly to counteract the allergic response. By constricting blood vessels and relaxing the airways, it quickly reverses the life-threatening symptoms of anaphylaxis. Administering epinephrine at the earliest signs of anaphylaxis is crucial, and anyone at risk of severe allergic reactions should carry an epinephrine auto-injector with them at all times.
While epinephrine can be a lifesaver, it is not a standalone solution. After administering epinephrine, it is vital to seek immediate medical attention. Anaphylaxis can have delayed recurrences, and further medical evaluation is necessary to ensure the individual’s safety and to address any lingering symptoms or complications.
In conclusion, allergic reactions are a widespread occurrence that varies in severity, from mild irritations to life-threatening anaphylaxis. Epinephrine is a lifesaving medication that can swiftly reverse the effects of anaphylaxis, but it should always be followed by professional medical care. Understanding the causes, symptoms, and proper use of epinephrine is essential for individuals with allergies and those around them to ensure swift and effective responses in the event of a severe allergic reaction.
To expand your knowledge on this subject, make sure to read on at this location: Epinephrine for First-aid Management of Anaphylaxis | Pediatrics …
Understanding Anaphylaxis
Anaphylaxis is a severe and rapid allergic reaction that can affect various body systems, including the skin, respiratory, gastrointestinal, and cardiovascular systems. It typically occurs within minutes to hours after exposure to an allergen, such as certain foods, insect stings, medications, or latex. Anaphylaxis can develop in individuals with known allergies or, in some cases, occur unexpectedly in people with no prior history of allergies.
Anaphylaxis is a medical emergency that demands immediate attention and treatment. When an individual experiences anaphylaxis, their immune system goes into overdrive, releasing a cascade of chemicals like histamines that can lead to a wide range of symptoms affecting different body systems.
The skin is often the first to show signs of anaphylaxis, with symptoms like hives, itching, and swelling. This outward manifestation serves as a warning sign, but it can quickly progress to more severe symptoms that impact the respiratory system. The airways may constrict, making it difficult to breathe, and the person might start wheezing, coughing, or experiencing a sensation of throat tightness. In severe cases, the person’s airway may become completely blocked, leading to a life-threatening situation.
Anaphylaxis can also involve the gastrointestinal system, causing symptoms like nausea, vomiting, abdominal pain, and diarrhea. These symptoms can be distressing and may exacerbate the overall sense of panic and discomfort during an episode of anaphylaxis.
Furthermore, the cardiovascular system can be severely affected. A rapid drop in blood pressure, known as anaphylactic shock, can occur. This can result in dizziness, loss of consciousness, and a weak or rapid pulse. The heart struggles to pump blood effectively, leading to decreased oxygen supply to vital organs, which can be fatal if not treated promptly.
What makes anaphylaxis even more unpredictable is that it can strike individuals with known allergies as well as those who have never experienced any allergic reactions before. This phenomenon, known as “idiopathic anaphylaxis,” underscores the importance of being prepared for potential allergens and having access to life-saving medications like epinephrine, which can counteract the effects of anaphylaxis.
The management of anaphylaxis involves not only treating the immediate symptoms but also identifying and avoiding the allergen that triggered the reaction. It is crucial for individuals with known allergies to carry an epinephrine auto-injector at all times and be trained in its proper use. Timely administration of epinephrine can significantly improve the chances of survival during an anaphylactic episode.
In summary, anaphylaxis is a complex and potentially life-threatening allergic reaction that can affect multiple body systems. Its sudden onset and unpredictable nature emphasize the importance of preparedness, awareness, and quick access to medical intervention, especially for individuals with allergies and those at risk of developing anaphylaxis.
For additional details, consider exploring the related content available here Management of Anaphylaxis at COVID-19 Vaccination Sites | CDC

Food Allergens
Some of the most common triggers for anaphylaxis include peanuts, tree nuts, shellfish, fish, milk, eggs, and soy.
Certainly, let’s expand on the idea of common triggers for anaphylaxis and explore some additional aspects related to this critical topic:
Food Allergies Beyond the Basics: While peanuts, tree nuts, shellfish, fish, milk, eggs, and soy are indeed some of the most common triggers for anaphylaxis, it’s essential to recognize that food allergies can extend beyond these items. Wheat, for example, is a common allergen, often leading to reactions ranging from mild hives to severe anaphylaxis. Moreover, many people are allergic to various fruits, vegetables, and spices, demonstrating the wide range of potential allergens.
Hidden Ingredients and Cross-Contamination: Food allergies can be particularly challenging because allergenic ingredients can hide in unexpected places. For instance, some sauces and dressings may contain hidden allergens, like soy or nuts. Cross-contamination in restaurants or food processing facilities is another significant concern. Individuals with food allergies must always remain vigilant and inquire about ingredients and preparation methods when dining out.
Emerging Allergens: In recent years, there have been reports of emerging allergens. One example is sesame, which has gained recognition as a significant allergen, leading to regulatory changes in food labeling requirements. Similarly, spices like cumin and coriander have been known to cause allergic reactions in some individuals, emphasizing the importance of staying informed about evolving allergen awareness.
Adult-Onset Allergies: While many allergies develop in childhood, it’s not uncommon for adults to develop new allergies later in life. This phenomenon is particularly intriguing and underscores the need for ongoing research into the triggers and mechanisms behind adult-onset allergies. For adults, this may necessitate adjusting to new dietary restrictions and being alert to potential allergens they previously tolerated.
Global Variation: The prevalence of food allergies can vary significantly by region and ethnicity. For instance, sesame allergies are more common in some Middle Eastern populations, while fish allergies are more prevalent in coastal areas. Understanding these regional variations can aid in healthcare practices, public awareness campaigns, and food labeling regulations.
Preventing Anaphylaxis: Anaphylaxis is a potentially life-threatening condition, so preventing allergic reactions is paramount. Individuals with known allergies should always carry epinephrine auto-injectors and educate those around them on how to use them. Additionally, raising awareness in schools, workplaces, and public spaces about allergen-free zones and proper response protocols is essential.
Advancements in Treatment: Researchers are continually exploring new treatment options for severe allergies, including immunotherapy and biologics. These approaches aim to desensitize individuals to allergens over time, potentially reducing the risk of anaphylaxis. Keeping abreast of these developments is crucial for both individuals with allergies and healthcare providers.
In summary, while peanuts, tree nuts, shellfish, fish, milk, eggs, and soy are indeed common triggers for anaphylaxis, food allergies are a complex and evolving field. Understanding the broader context of food allergies, including hidden ingredients, emerging allergens, and regional variations, is vital for both individuals with allergies and the broader community to ensure safety and promote inclusivity.
Additionally, you can find further information on this topic by visiting this page: Epinephrine for First-aid Management of Anaphylaxis | Pediatrics …
Insect Stings
Stings from bees, wasps, hornets, and fire ants can lead to severe allergic reactions.
Stings from bees, wasps, hornets, and fire ants can lead to severe allergic reactions, emphasizing the importance of understanding and managing these insect encounters. These tiny creatures, while often harmless when left undisturbed, possess potent defense mechanisms that can pose significant health risks to humans.
First and foremost, it’s crucial to recognize the distinct characteristics of these stinging insects and their habitats. Bees are generally non-aggressive and only sting when they feel threatened or provoked. Their stings can be painful but are typically less likely to trigger severe allergies. On the other hand, wasps, hornets, and fire ants are more aggressive and may sting even without provocation, making them potentially riskier.
Understanding the signs and symptoms of an allergic reaction to insect stings is vital. Allergic reactions can range from mild swelling, itching, and redness at the sting site to more severe symptoms such as difficulty breathing, hives, dizziness, and even anaphylaxis – a life-threatening condition that requires immediate medical attention. People who have experienced severe reactions in the past or have known allergies to insect stings should carry epinephrine auto-injectors (e.g., EpiPen) and know how to use them.
Prevention is key when it comes to insect stings. Wearing protective clothing when spending time in areas where stinging insects are prevalent, such as beekeeping suits or thick clothing, can help reduce the risk of stings. Avoiding bright-colored clothing and perfumed products can also make you less attractive to these insects. Keep food and sugary beverages covered when outdoors to deter wasps and hornets.
Educating oneself and others about the different types of stinging insects and their behaviors can go a long way in minimizing encounters and the potential for allergic reactions. Additionally, maintaining a clean outdoor environment by disposing of trash properly and sealing potential nesting sites can help reduce the presence of these insects near homes and recreational areas.
In cases of a known allergy or a history of severe reactions, it’s crucial to work closely with a healthcare provider to develop a personalized allergy management plan. This plan may include allergy testing, immunotherapy (allergy shots), and education on how to respond in the event of a sting. Furthermore, individuals with allergies should wear medical alert bracelets or carry identification specifying their allergy to ensure prompt and appropriate medical care in case of an emergency.
In summary, while the risk of severe allergic reactions from stings by bees, wasps, hornets, and fire ants is real, knowledge, preparedness, and prevention strategies can significantly mitigate these risks. By understanding the behavior of these insects, recognizing allergic reactions, and taking appropriate precautions, individuals can enjoy the outdoors safely and minimize the impact of these tiny but potentially dangerous creatures on their lives.
Looking for more insights? You’ll find them right here in our extended coverage: Allergies to bites and stings – Better Health Channel

Medications
Certain medications, such as antibiotics (e.g., penicillin), nonsteroidal anti-inflammatory drugs (NSAIDs), and intravenous contrast dyes, can trigger anaphylaxis.
The connection between certain medications and anaphylaxis is a critical aspect of understanding this severe allergic reaction. While medications are designed to treat various medical conditions and improve our health, it’s important to be aware that they can sometimes trigger severe allergic responses in some individuals.
Antibiotics: Antibiotics like penicillin, which are commonly prescribed to combat bacterial infections, are notorious for their potential to trigger allergic reactions. Penicillin and related antibiotics contain specific proteins that can stimulate an immune response in some people. When this response escalates into anaphylaxis, it becomes a medical emergency. It’s essential for healthcare providers to take a thorough medical history to identify individuals with known penicillin allergies and prescribe alternative antibiotics when necessary.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs are widely used for pain relief and reducing inflammation in conditions such as arthritis and headaches. Common examples include ibuprofen and aspirin. Though generally safe for many people, some may experience allergic reactions ranging from mild skin rashes to severe anaphylaxis. It’s vital to be cautious when taking NSAIDs, especially if you have a history of allergic reactions to these medications. Consult your healthcare provider for alternative pain management options.
Intravenous Contrast Dyes: Intravenous contrast dyes are used in medical imaging procedures like CT scans or angiograms to enhance the visibility of blood vessels and tissues. These dyes contain iodine, which can trigger allergic reactions in some individuals. Although severe reactions are relatively rare, they can include symptoms like hives, difficulty breathing, and, in rare cases, anaphylaxis. Patients undergoing procedures involving contrast dyes should inform their healthcare providers of any previous allergic reactions or iodine sensitivities.
Other Medications: While antibiotics, NSAIDs, and contrast dyes are common culprits, it’s essential to recognize that anaphylactic reactions can potentially occur with other medications too. It’s not limited to these categories. Any medication has the potential to cause allergic reactions in susceptible individuals. If you suspect you may be allergic to a medication or have experienced an allergic reaction in the past, inform your healthcare provider, and they can explore alternative treatments or perform allergy testing as needed.
In summary, certain medications, including antibiotics, NSAIDs, and contrast dyes, have the potential to trigger anaphylaxis in individuals with allergies or sensitivities. It’s crucial for both patients and healthcare providers to be vigilant and proactive in identifying and addressing medication allergies to ensure patient safety and well-being. This includes taking a thorough medical history, conducting allergy testing when necessary, and having an emergency action plan in place for individuals at risk of anaphylaxis due to medication allergies.
You can also read more about this here: What is Epinephrine? | Allergy & Asthma Network

Latex
People with latex allergies can experience anaphylaxis when exposed to latex products, such as gloves or medical devices.
Latex allergies represent a significant and often overlooked aspect of anaphylaxis, as exposure to latex-containing products can trigger severe allergic reactions in susceptible individuals. Latex, derived from the sap of rubber trees, is a common material used in various everyday items, particularly in healthcare settings. People with latex allergies face unique challenges and risks when it comes to anaphylaxis.
Latex anaphylaxis can occur in response to direct contact with latex products, such as gloves, condoms, or medical devices like catheters and syringe plungers. It’s not just the natural rubber latex itself that poses a risk; some individuals may also react to the proteins present in latex products, which are released into the air as a fine powder when latex is used or handled. Inhalation of these airborne latex particles can lead to respiratory symptoms and anaphylactic reactions in sensitive individuals.
The symptoms of latex-induced anaphylaxis can be similar to those of anaphylaxis caused by other allergens, including skin reactions like hives and itching, respiratory symptoms like wheezing and difficulty breathing, gastrointestinal issues such as abdominal pain and vomiting, and cardiovascular symptoms like a rapid or weak pulse. In severe cases, the allergic reaction can progress rapidly and lead to anaphylactic shock, which is a life-threatening condition.
One of the challenges in managing latex allergies is the ubiquity of latex-containing products in healthcare settings. Patients, as well as healthcare workers, may come into contact with latex during medical procedures, increasing the risk of exposure. Therefore, it’s crucial for individuals with latex allergies to communicate their allergy status to healthcare providers to ensure latex-free alternatives are used during medical procedures and examinations.
In recent years, efforts have been made to reduce latex exposure in healthcare settings, with many facilities adopting latex-free policies and using latex alternatives. These changes have helped mitigate the risk of latex-induced anaphylaxis in healthcare environments.
Moreover, individuals with known latex allergies should take proactive steps to avoid latex-containing products in non-medical settings as well. This includes checking product labels, notifying hairdressers or tattoo artists about their latex allergy, and choosing latex-free alternatives for everyday items like gloves, balloons, and household items.
In conclusion, latex allergies can lead to anaphylaxis when individuals are exposed to latex products. The airborne latex proteins released during use can pose a particular risk, making it important for people with latex allergies to be vigilant about their exposure and communicate their allergy status in healthcare settings. Education and awareness about latex allergies, as well as the availability of latex-free alternatives, are crucial in preventing and managing these potentially life-threatening allergic reactions.
Should you desire more in-depth information, it’s available for your perusal on this page: Adrenaline (epinephrine) for the treatment of anaphylaxis with and …

Symptoms of Anaphylaxis
Anaphylaxis symptoms can vary in severity but often progress rapidly. Common signs and symptoms include:
Certainly, let’s expand on the idea of anaphylaxis symptoms and delve into the varying severity of these symptoms, potential triggers, and the importance of prompt recognition and treatment:
Variability in Anaphylaxis Symptoms: Anaphylaxis is a highly unpredictable condition, and its symptoms can vary widely in severity and presentation from person to person. While some individuals may experience milder symptoms initially, others may rapidly progress to severe reactions. This variability can make it challenging to identify anaphylaxis, emphasizing the need for heightened awareness.
Common Signs and Symptoms:
Skin Reactions: Many anaphylactic reactions begin with skin symptoms such as itching, hives (urticaria), and flushing. These visible signs often serve as early indicators of an allergic response.
Respiratory Distress: Anaphylaxis can quickly affect the respiratory system. Mild symptoms may include a scratchy throat or nasal congestion, while more severe cases can lead to wheezing, coughing, difficulty breathing, or a sensation of throat tightening (known as laryngeal edema). These respiratory symptoms can escalate rapidly and are a hallmark of severe anaphylaxis.
Gastrointestinal Disturbances: Some individuals may experience nausea, vomiting, abdominal pain, or diarrhea during anaphylactic reactions. These symptoms can contribute to overall discomfort and dehydration in severe cases.
Cardiovascular Changes: Anaphylaxis can cause a drop in blood pressure (hypotension) and an increase in heart rate (tachycardia). These cardiovascular changes are particularly concerning as they can lead to shock, loss of consciousness, or cardiac arrest if not promptly addressed.
Mental Confusion: As anaphylaxis progresses, some individuals may experience confusion, agitation, or a sense of impending doom. These neurological symptoms are indicative of systemic involvement and the need for immediate medical intervention.
Swelling (Angioedema): Alongside hives, some individuals may develop swelling, particularly in the face, lips, tongue, or throat. Swelling of the throat can be particularly dangerous as it can obstruct the airway.
Triggers and Allergens: Anaphylaxis can be triggered by various allergens beyond the commonly recognized food allergens mentioned earlier. Common triggers include insect stings (e.g., bee or wasp stings), medications (e.g., antibiotics, non-steroidal anti-inflammatory drugs), latex, and even exercise-induced anaphylaxis. Understanding one’s specific triggers is crucial for managing and preventing anaphylactic reactions.
Importance of Prompt Recognition and Treatment: Recognizing the signs and symptoms of anaphylaxis is critical for swift action. Delayed treatment can result in a life-threatening situation. If anaphylaxis is suspected, immediate steps should be taken, including:
- Administering epinephrine via an auto-injector if available.
- Calling emergency services (911 in the United States) for immediate medical assistance.
- Lying down with legs elevated to help maintain blood flow.
- Monitoring vital signs (heart rate, breathing, and blood pressure) while waiting for medical help.
In conclusion, anaphylaxis symptoms can range from mild to severe and may progress rapidly. Understanding the common signs and triggers, as well as the importance of quick recognition and treatment, is crucial for individuals with allergies and those around them to ensure the best possible outcome in case of anaphylactic reactions.
For additional details, consider exploring the related content available here Anaphylaxis: Emergency treatment – UpToDate
Skin
Itching, hives, and a flushed or pale appearance.
Itching, hives, and a flushed or pale appearance are common physical manifestations of an allergic reaction, and understanding these symptoms is crucial for early recognition and appropriate response.
Itching: Itching is often one of the earliest signs of an allergic reaction. It can be localized at the site of the allergen exposure, such as the area around an insect sting or where a certain substance touched the skin. However, itching can also be generalized, affecting larger areas of the body. This intense itching sensation can be distressing and uncomfortable, prompting individuals to scratch, which may exacerbate the reaction and potentially introduce infections.
Hives (Urticaria): Hives are raised, red or pink welts that can appear anywhere on the skin. They often have a defined border and may vary in size from small dots to large patches. Hives can be extremely itchy and may come and go rapidly. They are a result of the release of histamine and other chemicals in response to the allergen. While hives are usually associated with allergic reactions, they can also occur due to non-allergic causes, such as stress or certain medications.
Flushed Appearance: A flushed or red appearance of the skin can indicate increased blood flow and dilation of blood vessels in response to the allergen-triggered release of histamine. This redness is often seen in conjunction with itching and hives and may be particularly noticeable in individuals with fair skin. On the other hand, some people may experience a pale appearance, which can be a sign of blood pressure drop or shock, a severe allergic reaction known as anaphylaxis.
Recognizing these physical symptoms is essential for prompt action. While itching and hives may be manageable with over-the-counter antihistamines, a pale or flushed appearance, especially when accompanied by other symptoms like difficulty breathing, swelling of the face and throat, and a rapid heartbeat, should be treated as a medical emergency. Anaphylaxis can progress rapidly and can be life-threatening without immediate administration of epinephrine and emergency medical attention.
It’s also worth noting that allergic reactions can manifest differently from person to person, and the severity can vary. Some individuals may only experience mild itching and hives, while others may quickly progress to more severe symptoms. Therefore, it’s crucial to take any allergic reaction seriously and seek appropriate medical guidance if you suspect an allergy or if the reaction is severe or worsens over time. Being aware of these symptoms and understanding how to respond can make a significant difference in managing allergic reactions safely and effectively.
Explore this link for a more extensive examination of the topic: Management of Anaphylaxis at COVID-19 Vaccination Sites | CDC
Respiratory
Shortness of breath, wheezing, coughing, and a feeling of throat tightness or swelling.
The symptoms of anaphylaxis can be truly frightening, and among the most distressing are those related to the respiratory system. When anaphylaxis strikes, it can have a swift and severe impact on a person’s ability to breathe, making it crucial to understand these respiratory symptoms:
Shortness of Breath: This is often one of the earliest signs of anaphylaxis. Individuals may suddenly feel as though they cannot take in enough air. This sensation of breathlessness can be terrifying and is typically accompanied by anxiety and restlessness. As the allergic reaction progresses, this symptom can worsen rapidly, underscoring the urgency of the situation.
Wheezing: Wheezing is a high-pitched, whistling sound that occurs when a person breathes, particularly during exhalation. It results from the narrowing of the airways due to muscle contractions and swelling, a hallmark of anaphylactic reactions. Wheezing is not only distressing for the person experiencing it but is also a clear sign that the airway is compromised.
Coughing: Coughing is another common respiratory symptom in anaphylaxis. It’s a reflexive response to the irritation and inflammation of the airways. The cough can be persistent and may worsen as the airway continues to narrow.
Feeling of Throat Tightness or Swelling: Perhaps one of the most alarming symptoms is the sensation of throat tightness or swelling, known as “throat constriction.” This occurs as the allergic response causes the tissues in the throat to swell, potentially leading to complete airway obstruction. It’s essential to recognize this symptom as a medical emergency and act swiftly.
These respiratory symptoms of anaphylaxis are the body’s way of signaling that it is in distress and requires immediate intervention. The constriction and swelling of the airways can rapidly progress to a point where breathing becomes impossible, leading to unconsciousness and, ultimately, death if left untreated.
Administering epinephrine and calling for emergency medical assistance are critical steps when these symptoms manifest. Epinephrine works to relax the muscles around the airways and reduce swelling, rapidly restoring normal breathing. However, it’s not a long-term solution, and individuals experiencing anaphylaxis should still seek medical evaluation to address the underlying cause and ensure their overall well-being.
In conclusion, the respiratory symptoms of anaphylaxis, including shortness of breath, wheezing, coughing, and throat tightness or swelling, are some of the most frightening and life-threatening aspects of this severe allergic reaction. Recognizing these symptoms and responding promptly with epinephrine and emergency medical care is essential for preventing the progression of anaphylaxis and saving lives.
For a comprehensive look at this subject, we invite you to read more on this dedicated page: Lesson of the week: Adrenaline given outside the context of life …

Cardiovascular
Rapid or weak pulse, drop in blood pressure, and dizziness.
The combination of a rapid or weak pulse, a drop in blood pressure, and dizziness is a critical cluster of symptoms that often signifies a severe medical emergency, such as anaphylactic shock or other life-threatening conditions. Let’s explore these symptoms further:
Rapid or Weak Pulse: A pulse is the rhythmic expansion and contraction of the arteries as blood is pumped through the body by the heart. In anaphylaxis and other medical emergencies, the pulse rate can change dramatically. A rapid pulse, medically known as tachycardia, is when the heart beats too fast. This can occur as the body tries to compensate for decreased blood flow by pumping more rapidly. On the other hand, a weak or thready pulse is when the pulse is difficult to detect or feels faint. This can result from a drop in blood pressure, reduced cardiac output, or constriction of blood vessels.
Drop in Blood Pressure: A sudden drop in blood pressure, medically referred to as hypotension, is a grave concern. It can occur for various reasons, including severe allergic reactions, anaphylaxis, heart conditions, or other medical emergencies. When blood pressure falls significantly, vital organs may not receive adequate blood and oxygen, leading to organ dysfunction and damage. This drop in blood pressure is especially dangerous if it progresses to a state of shock, which can be life-threatening.
Dizziness: Dizziness is a common symptom experienced when there is a sudden drop in blood pressure or when the brain doesn’t receive enough blood and oxygen. It often manifests as lightheadedness, feeling unsteady, or a sensation that the world is spinning. In medical emergencies like anaphylaxis, dizziness can be accompanied by confusion, altered consciousness, or loss of consciousness if the drop in blood pressure is severe.
These symptoms are indicative of a critical imbalance in the body’s cardiovascular system. In cases of anaphylaxis, they can result from the body’s extreme response to allergens, including the release of histamines, which cause blood vessels to dilate, leading to a drop in blood pressure. The rapid heart rate is a compensatory mechanism aimed at maintaining blood flow to vital organs.
Prompt recognition and intervention are crucial when these symptoms are present. In the case of anaphylaxis, the immediate administration of epinephrine (adrenaline) is the standard treatment to counteract the severe allergic reaction, stabilize blood pressure, and alleviate symptoms. Anyone witnessing or experiencing these symptoms should seek emergency medical assistance immediately, as they may require advanced medical interventions and monitoring to prevent life-threatening complications.
In conclusion, the presence of a rapid or weak pulse, a drop in blood pressure, and dizziness are critical signs that should never be ignored. They often indicate a severe medical emergency that necessitates immediate medical attention and intervention to prevent further complications and ensure the best possible outcome for the affected individual.
To delve further into this matter, we encourage you to check out the additional resources provided here: Anaphylaxis: Emergency treatment – UpToDate

Other
Anxiety, confusion, loss of consciousness, and a sense of impending doom.
Certainly, let’s expand on the idea of anxiety, confusion, loss of consciousness, and a sense of impending doom in the context of various medical conditions and situations where these symptoms may manifest:
Anxiety in Mental Health: Anxiety is a common mental health condition characterized by excessive worry, fear, or unease. It can range from mild to severe and may lead to physical symptoms like trembling, sweating, and rapid heartbeat. Anxiety disorders, such as generalized anxiety disorder (GAD) or panic disorder, often involve persistent and intense feelings of anxiety. In severe cases, panic attacks can induce a profound sense of impending doom, making it difficult for individuals to function.
Confusion in Neurological Disorders: Confusion can be a prominent symptom in various neurological conditions. Alzheimer’s disease, for instance, is a progressive neurodegenerative disorder characterized by memory loss and cognitive decline, leading to confusion and disorientation. Acute neurological issues like strokes or head injuries can also result in confusion due to damage to the brain.
Loss of Consciousness in Syncope: Syncope, commonly known as fainting, is a sudden loss of consciousness. It can occur for various reasons, including low blood pressure, dehydration, emotional stress, or sudden changes in position. The sensation of impending doom is sometimes reported just before syncope, likely due to the body’s response to decreased blood flow to the brain.
Sense of Impending Doom in Medical Emergencies: The feeling of impending doom can be a characteristic feature in various acute medical emergencies. For example, individuals experiencing a heart attack often describe a profound sense of impending doom due to the severe chest pain and the fear of a life-threatening event. In severe allergic reactions (anaphylaxis), a sense of impending doom can arise alongside other symptoms, emphasizing the urgency of medical intervention.
Hypoxia and Impending Doom: In situations where oxygen levels in the body are critically low, such as in severe respiratory distress or during high-altitude climbing without proper acclimatization, individuals may experience a strong sense of impending doom. This feeling can result from the body’s desperate need for oxygen and serves as a survival instinct, urging the individual to seek help or oxygen immediately.
Psychological and Emotional Responses: The feelings of anxiety, confusion, and impending doom are not limited to physical conditions alone. Traumatic events, such as accidents or natural disasters, can trigger these emotional responses in people as they grapple with fear, uncertainty, and the overwhelming nature of the situation.
Treatment and Support: In all these scenarios, recognizing these symptoms is crucial for timely intervention and support. Medical professionals are trained to assess and address these symptoms appropriately. Moreover, emotional and psychological support is essential for individuals experiencing these distressing feelings, whether due to medical conditions or external stressors.
In summary, anxiety, confusion, loss of consciousness, and a sense of impending doom can manifest in various medical, psychological, and emergency situations. Understanding the context and potential causes of these symptoms is vital for appropriate responses, interventions, and support to ensure the well-being and safety of individuals experiencing them.
Don’t stop here; you can continue your exploration by following this link for more details: Safety of epinephrine for anaphylaxis in the emergency setting – PMC
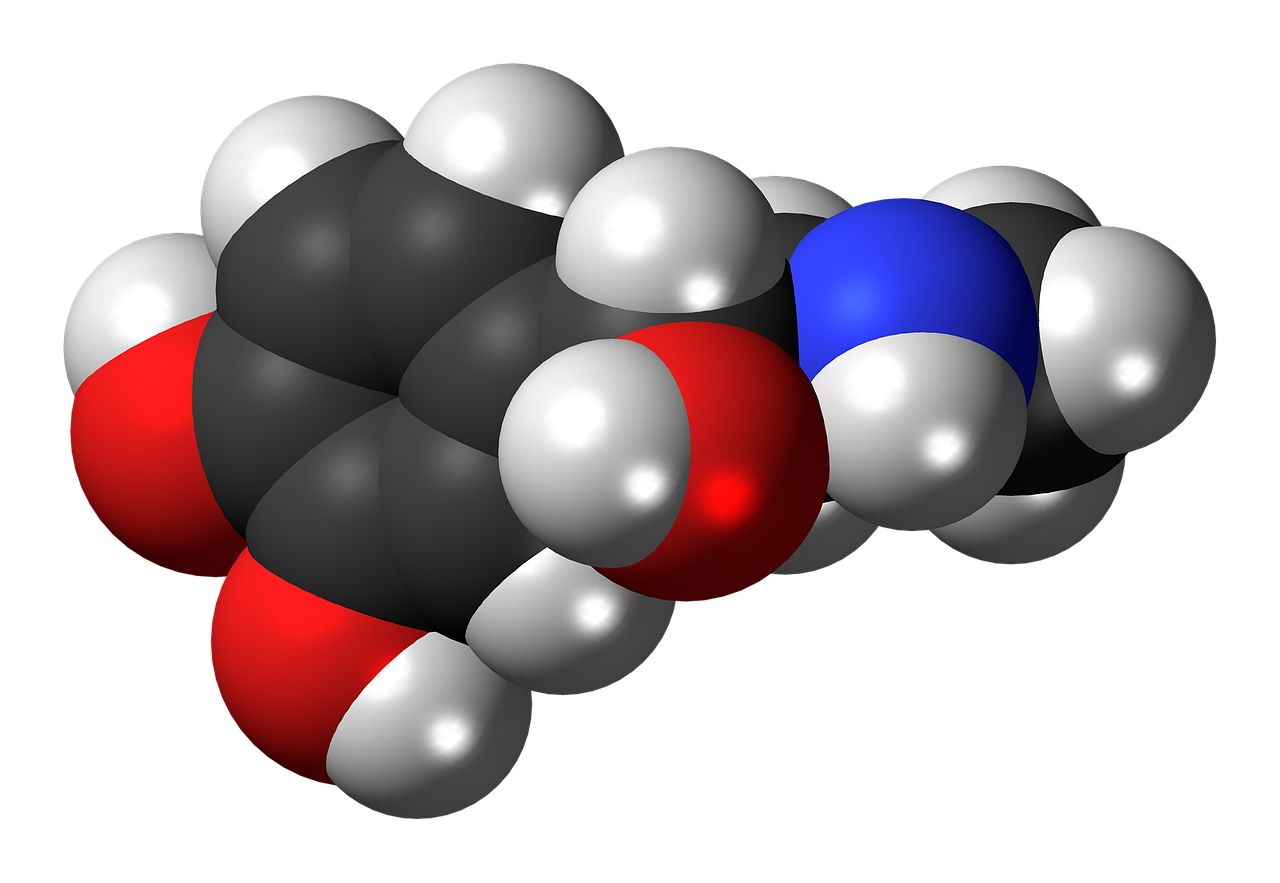
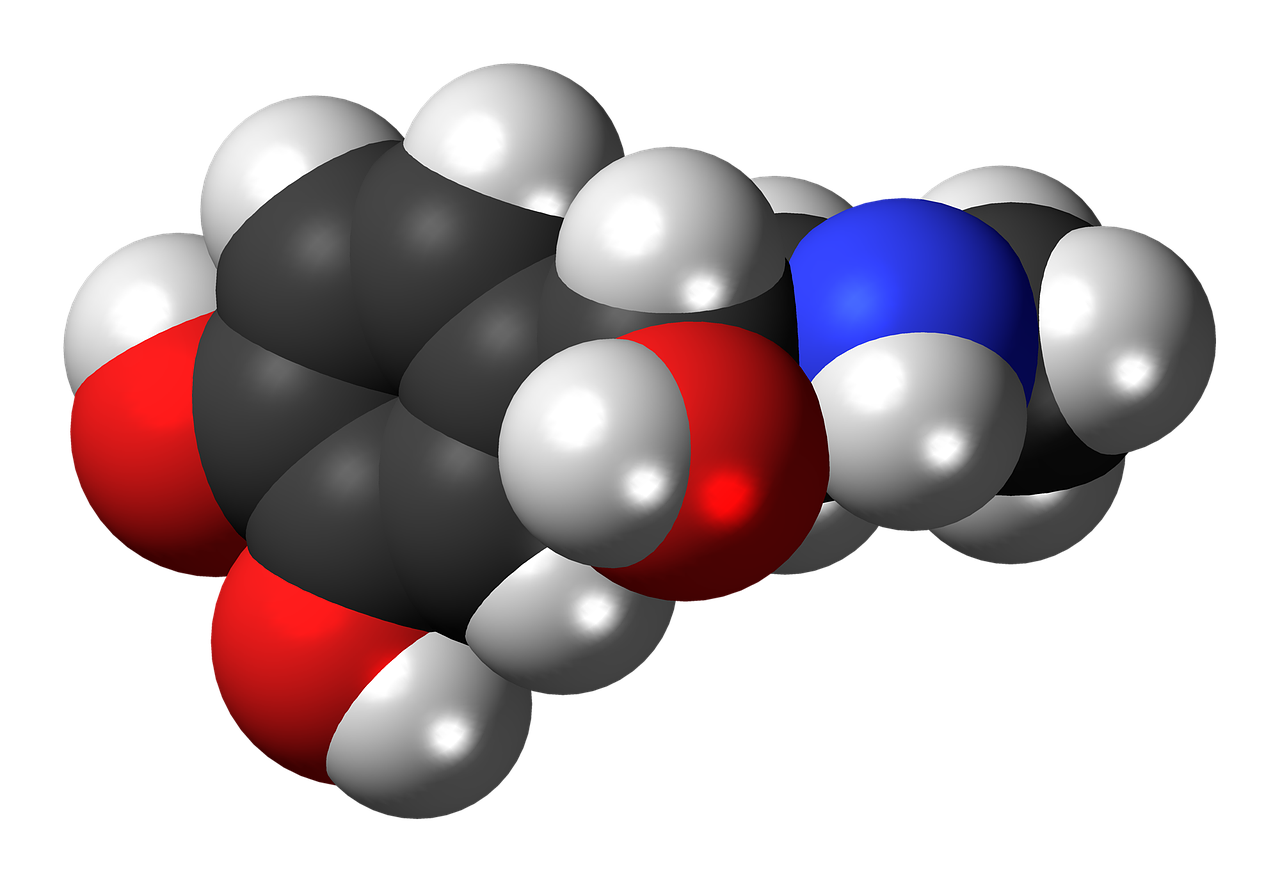
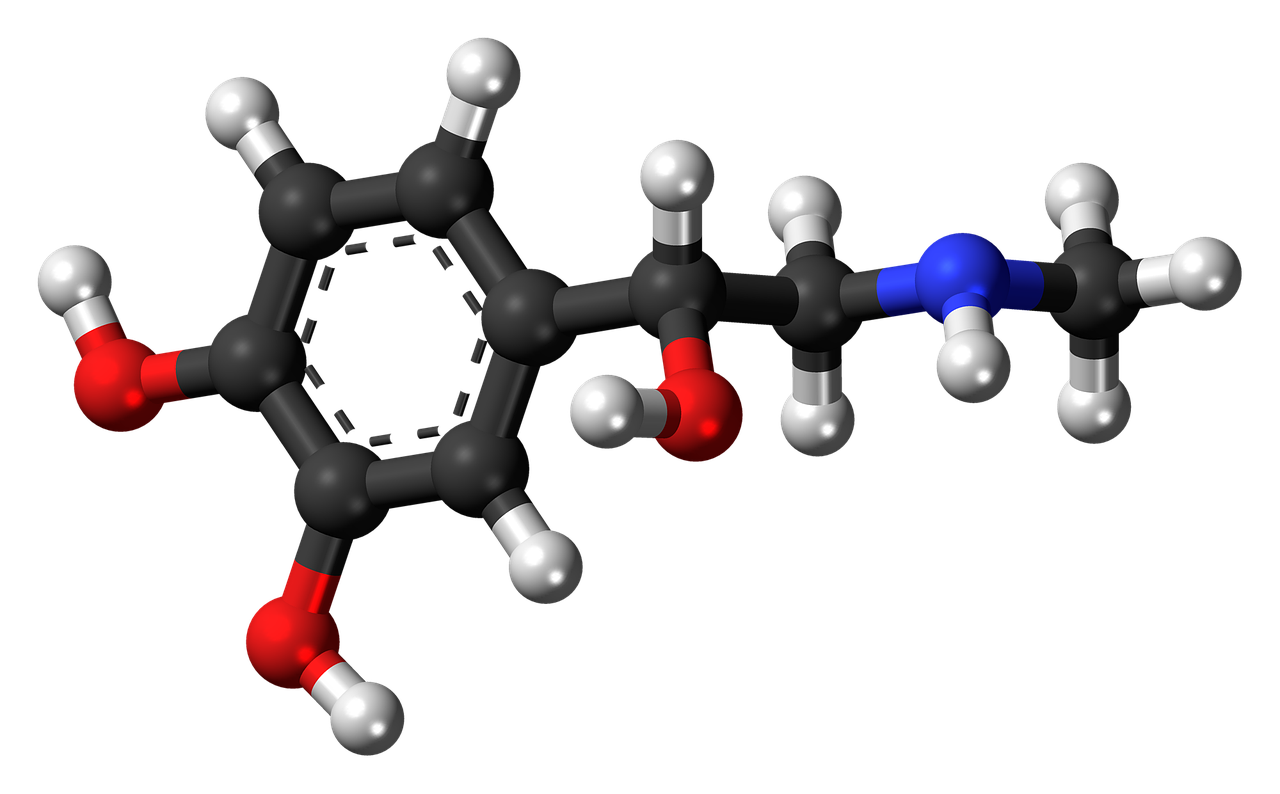
Epinephrine: The Lifesaving Medication
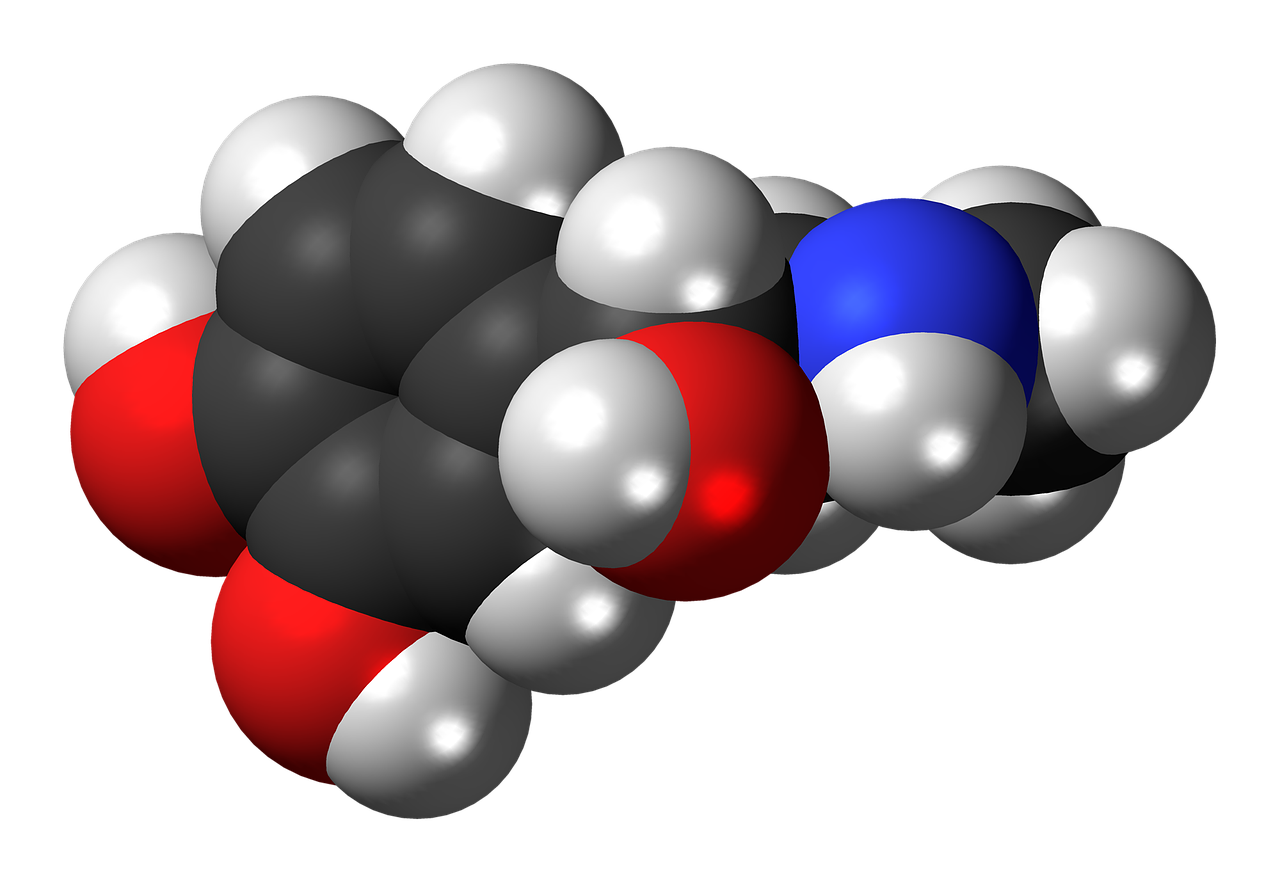
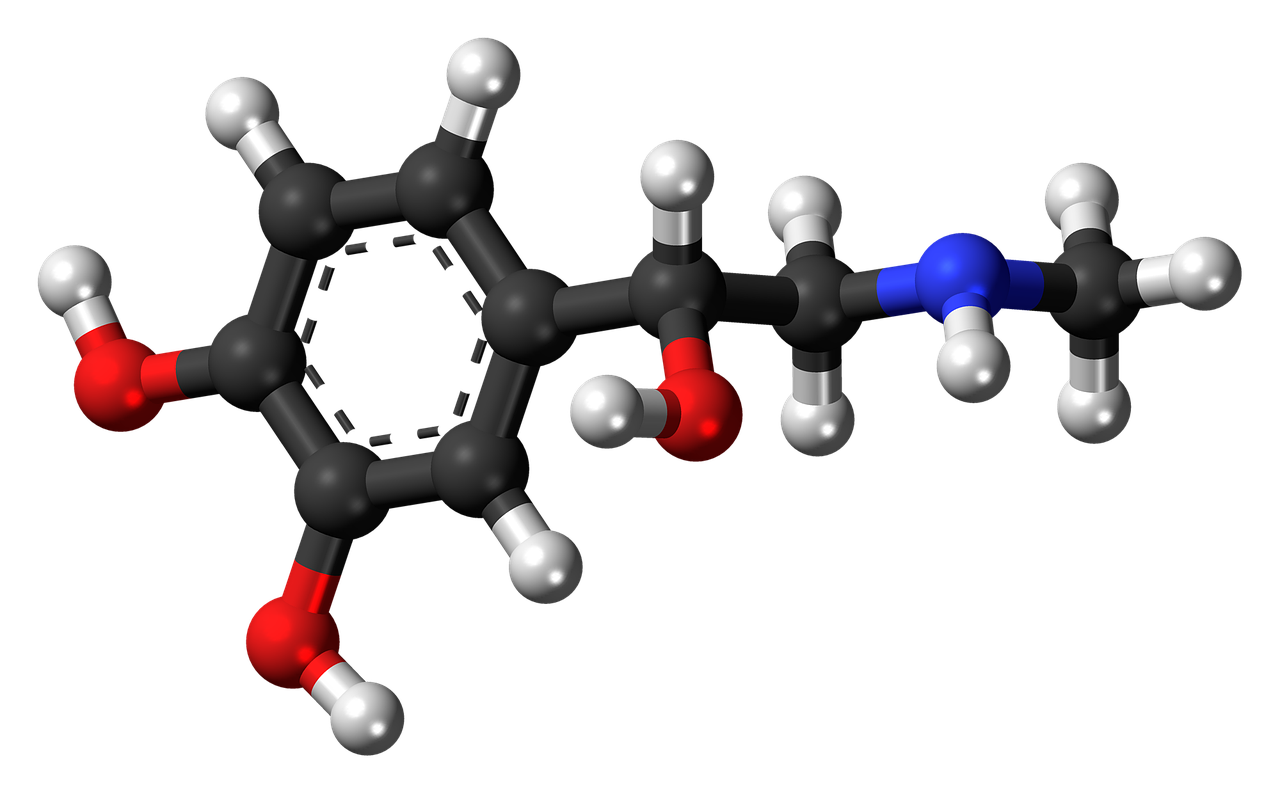
Epinephrine is a medication that can reverse the severe symptoms of anaphylaxis and prevent a life-threatening situation from worsening. It works by constricting blood vessels, increasing heart rate, and relaxing airway muscles, which helps counteract the allergic reaction’s effects.
Epinephrine, often referred to as an adrenaline shot, is an indispensable medication in the management of severe allergic reactions, such as anaphylaxis. Its rapid and potent effects play a crucial role in reversing the life-threatening symptoms associated with these reactions. Here’s a more detailed look at how epinephrine works and why it is so vital:
Vasoconstriction: Epinephrine acts swiftly to constrict blood vessels throughout the body. This vasoconstriction helps combat one of the most dangerous effects of anaphylaxis: a sudden drop in blood pressure. During anaphylaxis, blood vessels can dilate rapidly, leading to a significant decrease in blood pressure. This can result in shock, which, if not promptly addressed, can be fatal. Epinephrine’s ability to constrict blood vessels counteracts this dangerous drop in blood pressure, helping to stabilize the cardiovascular system.
Increased Heart Rate: Another critical action of epinephrine is its capacity to increase heart rate or pulse. This is essential for maintaining blood circulation and oxygen delivery to vital organs, including the brain and heart. The rapid heart rate induced by epinephrine helps compensate for the cardiovascular challenges posed by anaphylaxis, ensuring that vital organs receive adequate oxygen and nutrients.
Relaxation of Airway Muscles: Epinephrine also has a bronchodilatory effect, meaning it relaxes the smooth muscles lining the airways. During anaphylaxis, these airway muscles can constrict, leading to difficulty breathing or even complete airway obstruction. By relaxing these muscles, epinephrine helps restore normal airflow and alleviate respiratory distress, a crucial aspect of managing anaphylaxis.
Anti-inflammatory Properties: Epinephrine may also have some anti-inflammatory properties, which can help reduce swelling and inflammation in the body. While it’s not the primary mechanism of action, this anti-inflammatory effect can be beneficial in alleviating symptoms like swelling and hives.
In summary, epinephrine’s multifaceted actions work in concert to counteract the severe and potentially deadly effects of anaphylaxis. When administered promptly through an auto-injector (such as an EpiPen) by individuals experiencing anaphylactic symptoms or by trained healthcare professionals, epinephrine can be a lifesaver. However, it’s essential to seek immediate medical attention even after epinephrine administration because its effects may wear off, and further treatment and monitoring are often necessary to ensure a full recovery.
In cases of known severe allergies, individuals should carry an epinephrine auto-injector at all times, be trained in its proper use, and have an anaphylaxis action plan in place. By being prepared and understanding the critical role of epinephrine in managing anaphylaxis, individuals and caregivers can respond effectively to allergic emergencies, potentially saving lives.
For a comprehensive look at this subject, we invite you to read more on this dedicated page: Adrenaline (epinephrine) for the treatment of anaphylaxis with and …

Using Epinephrine
If you suspect someone is experiencing anaphylaxis or you are experiencing it yourself, follow these steps for using epinephrine:
If you suspect someone is experiencing anaphylaxis or if you are the one facing this potentially life-threatening situation, it is crucial to act swiftly and decisively. Anaphylaxis is a medical emergency, and administering epinephrine can be the difference between life and death. Here are the steps to follow for using epinephrine:
Stay Calm: In the midst of a severe allergic reaction, panic can set in quickly. It’s vital to remain as calm as possible. Panicking can worsen the situation by increasing heart rate and exacerbating anxiety, which may further constrict the airways.
Call 911: Your first action should be to dial 911 or your local emergency number. Anaphylaxis can escalate rapidly, and professional medical assistance is necessary. Even if you administer epinephrine, the person still requires immediate medical evaluation and treatment.
Locate the Epinephrine Auto-Injector: If you or the person experiencing anaphylaxis has been prescribed an epinephrine auto-injector, locate it immediately. These devices are typically carried in a purse, pocket, or designated case, so they are easily accessible in case of an emergency.
Read Instructions: Familiarize yourself with the instructions on the epinephrine auto-injector. These instructions may vary depending on the brand, so it’s essential to know how to use the specific device you have.
Prepare for Administration: Before administering epinephrine, it’s crucial to prepare for the injection. Make sure the correct end of the auto-injector is facing downward. Remove the safety cap or release any safety mechanism according to the instructions.
Select an Injection Site: The recommended injection site is the outer thigh. Ensure that the thigh is exposed, and there are no obstructions. Do not inject into the buttocks or a vein.
Administer the Epinephrine: Hold the auto-injector firmly against the thigh at a 90-degree angle. With a quick and forceful motion, push the injector against the thigh until you hear a click. Hold it in place for several seconds to ensure all the medication is delivered.
Dispose of the Injector Safely: After using the epinephrine auto-injector, follow local guidelines for safe disposal. Some devices have built-in mechanisms for covering the needle to prevent accidental needlesticks.
Seek Medical Attention: Epinephrine is not a cure for anaphylaxis; it provides temporary relief. After administering epinephrine, it is vital to seek immediate medical attention. The symptoms of anaphylaxis can sometimes return or worsen, making professional evaluation and treatment essential.
Monitor the Person: While waiting for emergency responders to arrive, stay with the person who received epinephrine. Keep them in a comfortable position, ideally lying down with their legs elevated to help improve blood flow.
Remember that using epinephrine is a life-saving measure, and hesitation can have dire consequences during an anaphylactic episode. Knowing how to use an epinephrine auto-injector and acting promptly can greatly improve the chances of a positive outcome. Additionally, once the situation is stabilized, it’s crucial to follow up with healthcare providers to identify the cause of the allergic reaction and develop a plan to prevent future occurrences.
To expand your knowledge on this subject, make sure to read on at this location: What is Epinephrine? | Allergy & Asthma Network

Call 911
Even if you administer epinephrine, it’s crucial to seek immediate medical help.
Administering epinephrine is a critical and potentially life-saving step in the management of severe allergic reactions and anaphylaxis. However, it’s essential to understand that epinephrine is not a standalone solution but rather a first-line treatment that provides temporary relief and buys valuable time for the individual in distress. Here’s why seeking immediate medical help remains paramount, even after administering epinephrine:
Short-Term Relief: Epinephrine acts rapidly to counteract the effects of anaphylaxis by reversing symptoms like airway constriction, low blood pressure, and hives. It can be a lifesaver, but its effects are temporary and may wear off within 15-20 minutes. In some cases, a second dose of epinephrine may be necessary if the symptoms persist or recur.
Underlying Causes: Epinephrine addresses the immediate symptoms but doesn’t treat the underlying cause of the allergic reaction. Identifying and managing the allergen exposure is crucial to prevent a recurrence of the reaction. For instance, if the trigger was a food allergen, it’s essential to eliminate that allergen from the individual’s diet and seek guidance from an allergist for long-term management.
Monitoring and Further Treatment: Anaphylaxis can have delayed or biphasic reactions, where symptoms may recur or worsen hours after the initial exposure. Therefore, individuals who have received epinephrine must be closely monitored in a medical setting for several hours to ensure that their condition remains stable and to address any potential complications. Additional treatments, such as antihistamines, corticosteroids, and intravenous fluids, may be necessary to manage ongoing symptoms and stabilize blood pressure.
Preventing Future Episodes: Seeking immediate medical help allows healthcare professionals to conduct a comprehensive evaluation and develop a personalized management plan for the individual. This plan may include allergy testing, allergen avoidance strategies, and the prescription of an epinephrine auto-injector for future emergencies. Education on recognizing and managing allergic reactions is also crucial for the individual and their caregivers.
Documentation and Communication: Seeking medical help ensures that the allergic reaction is documented in the individual’s medical records. This information is valuable for healthcare providers, especially if the individual requires follow-up care or encounters future allergic reactions. It also aids in communication between healthcare professionals, ensuring a consistent and informed approach to the individual’s care.
In summary, while administering epinephrine is a crucial initial response to anaphylaxis, it’s only the beginning of the treatment process. Seeking immediate medical help is essential to provide comprehensive care, address the underlying causes, monitor for potential complications, and develop a long-term management plan. Anaphylaxis is a medical emergency that requires a coordinated and multidisciplinary approach to ensure the safety and well-being of the individual affected by it.
Additionally, you can find further information on this topic by visiting this page: Epinephrine Auto-Injector and Anaphylaxis

Administer Epinephrine
Use an epinephrine auto-injector, which is a device designed for easy use. Follow the instructions provided with the device and administer the injection into the outer thigh. Hold it in place for several seconds to ensure all the medication is delivered.
Certainly, let’s expand on the idea of using an epinephrine auto-injector for the treatment of severe allergic reactions and provide additional guidance on its proper administration:
1. Swift Action is Crucial: When faced with a severe allergic reaction, time is of the essence. Anaphylaxis can progress rapidly, affecting multiple body systems, including the respiratory and cardiovascular systems. Administering epinephrine promptly is the most effective way to counteract these life-threatening symptoms.
2. Understanding the Epinephrine Auto-Injector:
- The epinephrine auto-injector is a user-friendly, pre-filled device designed to deliver a precise dose of epinephrine, a life-saving medication that rapidly reverses the effects of anaphylaxis.
- Familiarize yourself with the specific brand and model of auto-injector you have, as instructions may vary slightly between different devices.
3. Following the Instructions:
- Always follow the instructions provided with your auto-injector. These instructions are typically clear and concise, featuring both written and visual guidance.
- Most auto-injectors have a safety cap that must be removed before use. Grasp the device firmly in your dominant hand, keeping your thumb and fingers away from the needle end.
4. Administering the Injection:
- Place the auto-injector against the outer thigh. This is the preferred injection site because it allows for rapid absorption of the medication into the bloodstream.
- Push the auto-injector firmly against the thigh until it clicks or triggers. The device is designed to work through clothing, so there’s no need to expose the skin.
5. Holding it in Place:
- After triggering the auto-injector, keep it in place against the thigh for several seconds, typically 5 to 10 seconds, depending on the specific device. This ensures that the full dose of epinephrine is delivered into the muscle.
- It’s natural to feel some resistance while holding the device against the thigh during the injection.
6. Seeking Immediate Medical Assistance:
- Epinephrine is not a substitute for professional medical care. After administering the epinephrine, call 911 (or your local emergency number) immediately. Anaphylaxis requires comprehensive medical evaluation and treatment.
- Even if the symptoms appear to improve after epinephrine administration, they can recur, so it’s essential to have medical professionals assess the situation.
7. Preparing for Additional Doses:
- In some cases, a single dose of epinephrine may not be sufficient to control severe anaphylaxis. Certain individuals may require additional doses or medical treatments. It’s advisable to have a backup auto-injector available if needed.
8. Educating Others:
- If you have severe allergies, make sure that family members, close friends, and those you frequently spend time with are familiar with the proper use of the epinephrine auto-injector. They should know where it’s kept and how to use it in case of an emergency.
In conclusion, knowing how to use an epinephrine auto-injector correctly and taking swift action when an allergic reaction occurs can be life-saving. Familiarize yourself with your specific device and always follow the provided instructions. Administering epinephrine promptly and seeking professional medical help are crucial steps in managing anaphylaxis effectively.
If you’d like to dive deeper into this subject, there’s more to discover on this page: The Emperor Has No Symptoms: The Risks of a Blanket Approach to …

Lie Down
If possible, lay the person down with their legs elevated to help improve blood flow.
“If possible, lay the person down with their legs elevated to help improve blood flow” is a valuable piece of advice when dealing with a person experiencing a severe allergic reaction or anaphylaxis. Expanding on this idea, let’s delve into why this position can be beneficial and provide some additional context:
Improved Blood Flow: Elevating the legs of the person experiencing anaphylaxis can help facilitate blood return to the heart. When a severe allergic reaction occurs, blood vessels may dilate (widen) excessively, causing blood to pool in the extremities. This can result in a significant drop in blood pressure, potentially leading to shock. Elevating the legs above heart level encourages the blood to flow back towards the core and vital organs, aiding in maintaining adequate blood pressure.
Reduced Swelling: Anaphylactic reactions often involve swelling, particularly in the face and throat. This swelling can contribute to airway constriction and breathing difficulties. Elevating the legs can help reduce swelling in the extremities, allowing the body to redirect resources to addressing the allergic reaction itself, which may include administering epinephrine.
Comfort and Calmness: Lying down with legs elevated can be more comfortable for the individual in distress. It also helps reduce the risk of fainting, which can occur due to low blood pressure during anaphylaxis. A comfortable and calm patient is more likely to cooperate and follow necessary treatment steps.
Prevention of Falling: In cases where the person feels lightheaded or dizzy due to the allergic reaction or epinephrine administration, lying down with legs elevated can prevent falls and further injury.
While elevating the legs is a useful intervention, it’s essential to remember that it should not delay the administration of epinephrine or seeking emergency medical assistance. Epinephrine is the primary and most critical treatment for anaphylaxis. If you or someone you are assisting is experiencing severe allergic symptoms, such as difficulty breathing, swelling of the face and throat, or a drop in consciousness, administer epinephrine immediately as prescribed and then seek emergency medical help. Elevating the legs can be done in conjunction with these actions to improve overall outcomes.
Furthermore, if the person loses consciousness or stops breathing, it is essential to begin CPR (cardiopulmonary resuscitation) if trained to do so until medical professionals arrive. Time is of the essence during anaphylaxis, so swift and appropriate action is vital in ensuring the best possible outcome for the individual in distress.
Explore this link for a more extensive examination of the topic: Medical Management of Vaccine Reactions in Adults in a …

Stay Calm
Encourage the person to remain as calm as possible to reduce anxiety, which can exacerbate symptoms.
Encouraging someone experiencing anaphylaxis to remain as calm as possible is not just a well-intentioned suggestion; it’s a crucial element of their immediate care. Anxiety can significantly exacerbate the symptoms of anaphylaxis and make the situation even more challenging to manage. Here’s why maintaining a sense of calm is essential:
Reduced Stress Response: Anxiety and fear trigger the body’s stress response, releasing hormones like cortisol and adrenaline. While epinephrine (adrenaline) is administered to counteract the allergic reaction, additional adrenaline released due to anxiety can intensify the already heightened physiological response. This can lead to an increased heart rate, elevated blood pressure, and potentially worsening symptoms.
Improved Breathing: Anxiety can cause rapid, shallow breathing or hyperventilation. In someone already experiencing shortness of breath due to anaphylaxis, this can compound the difficulty of breathing. Encouraging calmness and slower, deeper breaths can help maintain better oxygen exchange and minimize the risk of respiratory distress.
Better Mental Focus: Staying calm allows the person to think more clearly and communicate effectively. During an anaphylactic reaction, it’s crucial to relay information to healthcare providers or those assisting with the situation. This includes information about allergies, previous reactions, and any medications taken.
Reduction in Overall Stress: Anaphylaxis is a highly stressful event for both the affected individual and those around them. By encouraging calmness, you not only help the person experiencing the reaction but also create a more controlled and composed atmosphere for everyone involved. This can lead to more effective decision-making and action.
To promote a sense of calm during an anaphylactic episode:
Offer Reassurance: Let the person know that help is on the way and that you are there to support them.
Provide a Safe Environment: Ensure that the person is in a secure and comfortable position, which can help alleviate anxiety.
Distract and Divert: Engage them in conversation about non-anxiety-inducing topics, like their favorite hobbies or experiences. Diverting their attention can help reduce anxiety levels.
Avoid Overloading with Information: While it’s essential to gather information about allergies and previous reactions, try not to overwhelm the person with questions. Keep communication clear and concise.
Stay Positive and Supportive: Offer words of encouragement and let them know that they are not alone in facing this challenge. Reiterate that medical assistance is on the way.
By prioritizing a calm and composed approach in the face of anaphylaxis, you can contribute to a safer and more manageable environment during this medical emergency. Remember that anaphylaxis is a time-sensitive condition, so while maintaining calm is vital, prompt administration of epinephrine and seeking immediate medical attention should remain the primary focus.
Additionally, you can find further information on this topic by visiting this page: Insect Sting Allergy (for Parents) – Nemours KidsHealth
Wait for Medical Help
Even if the symptoms improve after epinephrine administration, it’s essential to wait for emergency medical responders to arrive. Anaphylaxis can sometimes have a delayed recurrence.
Waiting for emergency medical responders to arrive, even if the initial symptoms improve after epinephrine administration, is a vital precaution in managing anaphylaxis. The potential for a delayed recurrence or secondary reaction highlights the importance of continued medical supervision and preparedness:
Delayed Recurrence: Anaphylactic reactions can be unpredictable, and while epinephrine provides rapid relief by reversing the immediate symptoms, it doesn’t guarantee that the reaction is fully resolved. In some cases, anaphylaxis can have a biphasic or protracted course, with symptoms reoccurring or worsening hours after the initial exposure or treatment. These delayed reactions can be just as severe, if not more so, than the initial presentation.
Monitoring: Healthcare providers and emergency responders have the training and equipment to monitor the individual’s vital signs, including heart rate, blood pressure, and oxygen levels. They can closely observe the patient for any signs of a secondary reaction and intervene promptly if necessary. Additionally, they can assess the individual’s overall condition and provide additional treatments or medications as needed to ensure stability.
Advanced Medical Care: Beyond monitoring, emergency medical responders are equipped to provide advanced medical care in case of complications. This may include administering intravenous fluids, medications like antihistamines and corticosteroids, or other interventions tailored to the individual’s specific needs. Their expertise and resources are crucial in managing potential complexities associated with anaphylaxis.
Transport to a Healthcare Facility: If there is a delayed recurrence or any uncertainty about the individual’s condition, emergency responders can swiftly transport them to a hospital or healthcare facility. This ensures that the person receives continuous care and access to specialized medical expertise, should their condition deteriorate again. Hospitals are also equipped to perform diagnostic tests and further evaluations, if necessary.
Allergen Identification: During the assessment by emergency responders, efforts can be made to identify the specific allergen that triggered the anaphylactic reaction. This information is valuable for future avoidance strategies and allergen management. It can help the individual and their healthcare team develop a comprehensive plan to prevent future exposures.
In summary, the possibility of a delayed recurrence of anaphylaxis underscores the need to remain vigilant and prioritize the involvement of emergency medical responders. While epinephrine is a crucial first-line treatment, it is not a guarantee that the crisis is over. Waiting for professional medical assistance ensures ongoing monitoring, access to advanced care, and the potential identification of allergen triggers, all of which are essential for the individual’s safety and well-being in the face of this life-threatening condition.
Explore this link for a more extensive examination of the topic: Evidence update for the treatment of anaphylaxis – PMC

Preventing Anaphylaxis
Prevention is key to managing anaphylaxis. Here are some strategies to reduce the risk:
Certainly, let’s expand on the idea of prevention as a key element in managing anaphylaxis and explore various strategies and considerations to reduce the risk of severe allergic reactions:
1. Allergen Identification:
- The foundation of anaphylaxis prevention is identifying and understanding your specific allergens. This involves comprehensive allergy testing, often conducted by an allergist. Once you know your triggers, you can take targeted steps to avoid them.
2. Reading Labels and Ingredient Lists:
- For individuals with food allergies, diligent label reading is crucial. Food packaging should clearly list allergenic ingredients, making it easier to identify potential risks. Learning how to decipher ingredient lists and recognize hidden allergens is vital.
3. Communicate Allergies:
- Informing those around you about your allergies is essential. This includes friends, family, co-workers, school personnel, and restaurant staff. Effective communication helps create a supportive environment where everyone understands the seriousness of your allergies.
4. Food Allergy Management Plans:
- For children with food allergies, schools should have well-defined food allergy management plans in place. This includes educating staff, implementing allergen-free zones, and having emergency protocols for anaphylactic reactions.
5. Medication Availability:
- Carry prescribed medications with you at all times, especially if you have a known severe allergy. Epinephrine auto-injectors should be readily accessible, and you should be trained in their use.
6. Emergency Action Plans:
- Develop and share an anaphylaxis emergency action plan with your healthcare provider, family members, and caregivers. This plan should outline steps to take in the event of an allergic reaction.
7. Avoiding Cross-Contamination:
- If you have food allergies, take precautions to prevent cross-contamination in your kitchen and when dining out. This includes using separate utensils, cleaning surfaces thoroughly, and asking about food preparation methods in restaurants.
8. Insect Allergy Prevention:
- Individuals with insect allergies should take precautions when spending time outdoors. This may involve wearing protective clothing, using insect repellent, and being cautious around areas where stinging insects are common.
9. Medication Allergy Management:
- If you have medication allergies, make sure your healthcare providers are aware of them. Alternative medications can often be prescribed to avoid triggering allergic reactions.
10. Regular Allergy Checkups: – Stay connected with your allergist for regular checkups and updates on your allergies. They can provide guidance on managing allergies and may conduct retesting to monitor changes in your allergen sensitivities.
11. Travel Preparedness: – When traveling, research the local cuisine and medical facilities at your destination. Ensure you have an adequate supply of medications and carry necessary documentation regarding your allergies in case of emergencies.
12. Be Vigilant in Social Settings: – When dining with friends or attending social events, communicate your allergies to the host or restaurant staff. Being proactive in these situations can help prevent accidental exposures.
13. Stay Informed: – Continue to educate yourself about allergies, anaphylaxis, and emerging research. Staying informed allows you to adapt and incorporate the latest safety measures into your daily life.
In conclusion, managing anaphylaxis involves a proactive approach centered on prevention. By identifying allergens, communicating effectively, carrying necessary medications, and implementing practical strategies, individuals with allergies can significantly reduce the risk of severe allergic reactions and enjoy a safer and more confident lifestyle.
To delve further into this matter, we encourage you to check out the additional resources provided here: Anaphylaxis: Emergency treatment – UpToDate
Know Your Triggers
If you have known allergies, identify and avoid your triggers.
Identifying and avoiding your known allergy triggers is a fundamental step in managing allergies and preventing potentially serious or life-threatening reactions. Expanding on this idea, here are some essential considerations and strategies for effectively managing allergies:
Allergen Awareness: To effectively avoid allergens, you must first identify them. Work closely with an allergist or immunologist to determine the specific substances to which you are allergic. Allergy testing, including skin tests or blood tests, can help pinpoint these triggers accurately. Common allergens include pollen, dust mites, pet dander, certain foods, insect stings, and various medications.
Educate Yourself: Once you know your allergy triggers, take the time to educate yourself about where and how these allergens can be encountered. For example, if you’re allergic to pollen, understanding the pollen seasons in your region can help you plan outdoor activities accordingly. If you have food allergies, learn to read ingredient labels and ask about ingredients when dining out.
Allergen Avoidance Strategies: Depending on your specific allergies, there are various strategies to minimize exposure:
Environmental Allergens: For allergies like pollen, dust mites, or pet dander, consider using high-efficiency particulate air (HEPA) filters in your home, regularly cleaning and dusting, and keeping windows closed during peak pollen seasons. If you have pet allergies, create pet-free zones in your home.
Food Allergies: When dealing with food allergies, carefully read food labels and ask about ingredients when dining out. Inform friends, family, and caregivers about your food allergies, and consider carrying an allergy action plan or medical alert bracelet.
Insect Allergies: If you’re allergic to insect stings, take precautions when spending time outdoors, such as wearing protective clothing, using insect repellent, and avoiding sweet-smelling products that attract insects.
Emergency Action Plan: Develop an emergency action plan in consultation with your healthcare provider. This plan should outline the steps to take in case of an allergic reaction, including the proper use of epinephrine if prescribed. Ensure that your close contacts, such as family members, friends, or coworkers, are familiar with this plan and know how to assist you during an allergic emergency.
Regular Check-Ups: Schedule regular follow-up appointments with your allergist to monitor your allergies and discuss any changes in your condition. Allergies can evolve over time, and it’s essential to stay informed about your current allergen sensitivities.
Travel Considerations: When traveling, research the allergen exposure at your destination and plan accordingly. Pack necessary medications and allergy supplies, and be cautious when trying new foods or engaging in outdoor activities in unfamiliar environments.
Support Networks: Consider joining support groups or online communities for individuals with allergies. Sharing experiences and tips with others who have similar allergies can be invaluable in managing your condition.
In conclusion, identifying and avoiding your allergy triggers is a proactive and empowering approach to allergy management. By staying informed, taking preventative measures, and having a well-defined plan for managing allergic reactions, you can lead a more comfortable and healthier life while reducing the risk of severe allergic episodes. Consulting with healthcare professionals and staying vigilant in your allergen avoidance efforts are key to successful allergy management.
For additional details, consider exploring the related content available here Anaphylaxis: Symptoms & Treatment

Carry an Epinephrine Auto-Injector
If you have a history of severe allergies, your healthcare provider may prescribe an epinephrine auto-injector for you to carry at all times.
For individuals with a history of severe allergies, carrying an epinephrine auto-injector at all times becomes not just a precaution but a lifeline. This medical device is a critical component of their daily routine, offering a sense of security and readiness to counteract potentially life-threatening allergic reactions. Here’s why it’s essential for those with severe allergies to have an epinephrine auto-injector with them at all times:
Rapid Response: Anaphylaxis can strike suddenly and progress rapidly. When exposed to a known allergen, there may be only minutes to react before symptoms become severe. Having an epinephrine auto-injector on hand ensures immediate access to the life-saving medication, allowing for a rapid response that can make all the difference in managing the allergic reaction effectively.
Self-Administration: Epinephrine auto-injectors are designed for easy and quick self-administration. In a moment of crisis, individuals can use the device to inject epinephrine into their thigh without the need for medical expertise. This empowers them to take control of their health and potentially save their own life.
Peace of Mind: Knowing that an epinephrine auto-injector is readily available provides a significant psychological benefit. It reduces anxiety and fear associated with daily activities and exposure to potential allergens. This peace of mind is invaluable for individuals with severe allergies and their families.
Increased Mobility: Having an epinephrine auto-injector allows individuals to lead a more active and independent lifestyle. They can confidently participate in social events, dine out, travel, and engage in various activities, knowing they have the means to manage an allergic reaction if it occurs.
Preparedness for Unpredictable Allergen Exposure: Allergen exposure can be unpredictable, even for those who are diligent about avoiding triggers. Cross-contamination in food, insect encounters, or inadvertent exposure to allergens in public places can occur unexpectedly. Carrying an epinephrine auto-injector ensures preparedness for such unforeseen situations.
Protecting Against Recurrent Reactions: Anaphylactic reactions can sometimes recur or worsen, even after the initial administration of epinephrine. Carrying multiple auto-injectors or having access to immediate medical care is essential for addressing such scenarios.
Compliance with Medical Advice: Healthcare providers prescribe epinephrine auto-injectors for individuals with a history of severe allergies based on their medical assessment. Carrying and using the device as instructed by the healthcare provider is a responsible and medically recommended practice that demonstrates commitment to one’s health.
In conclusion, an epinephrine auto-injector is an indispensable tool for individuals with a history of severe allergies. It enables them to respond rapidly and effectively to anaphylactic reactions, reducing the risk of complications and potentially saving lives. Carrying this device at all times is not just a medical recommendation; it’s a practical and empowering strategy that enhances the quality of life for those living with severe allergies.
Looking for more insights? You’ll find them right here in our extended coverage: What factors affect the carriage of epinephrine auto-injectors by …
Wear Medical Alert Identification
Wearing a medical alert bracelet or necklace can inform others about your allergies in case you cannot communicate during an emergency.
Wearing a medical alert bracelet or necklace is a simple yet effective way to communicate vital information about your allergies, especially when you may be unable to communicate during an emergency. This small accessory can be a lifesaver in several ways:
Immediate Identification: During a severe allergic reaction, you might become disoriented, lose consciousness, or be too overwhelmed by symptoms to communicate effectively. A medical alert bracelet or necklace serves as an instant identifier for first responders, healthcare professionals, or bystanders, allowing them to quickly recognize that you have allergies and need special attention.
Allergy Specifics: These medical alert accessories can include essential information such as the specific allergens you’re allergic to, the severity of your allergies, and emergency contact details. This information provides immediate guidance to those assisting you, enabling them to take appropriate actions, including administering the right treatments or notifying your loved ones.
Avoiding Accidental Exposure: In non-emergency situations, a medical alert bracelet or necklace can also help prevent accidental exposure to allergens. For example, if you’re unconscious or unable to speak, medical professionals can check your accessory to ensure that they do not use latex gloves or administer medications that contain allergenic ingredients.
Enhancing Safety While Traveling: When you travel or visit new places, it can be challenging to communicate your allergies effectively due to language barriers or unfamiliarity with local healthcare systems. A medical alert accessory transcends language barriers and provides a universal signal for healthcare providers worldwide to exercise caution regarding your allergies.
Peace of Mind: Wearing a medical alert bracelet or necklace can provide you and your loved ones with peace of mind. It reassures you that even in the most dire circumstances, important medical information is readily available, increasing the chances of receiving appropriate care promptly.
Compliance with Medical Recommendations: Healthcare professionals often recommend medical alert accessories for individuals with severe allergies, especially those at risk of anaphylaxis. Wearing one demonstrates your commitment to following medical advice and taking proactive steps to manage your allergies responsibly.
Empowering Independence: For individuals with allergies, particularly children or elderly individuals, medical alert accessories can empower them to lead more independent lives. Caregivers and family members can rest easier knowing that the wearer has an added layer of safety.
In conclusion, wearing a medical alert bracelet or necklace is a practical and potentially life-saving measure for individuals with allergies. It provides a clear and immediate means of communication when you may be unable to speak or convey critical information during an emergency. This small accessory can make a significant difference in the quality of care you receive and enhance your overall safety, offering peace of mind to both you and your loved ones.
To delve further into this matter, we encourage you to check out the additional resources provided here: Food Allergy | Anaphylaxis | Food Allergies | MedlinePlus

Educate Others
Teach family members, friends, and close contacts how to recognize the signs of anaphylaxis and administer epinephrine if needed.
Certainly, let’s expand on the importance of educating family members, friends, and close contacts about anaphylaxis recognition and the proper administration of epinephrine:
1. Raising Awareness Saves Lives:
- Teaching those around you how to recognize the signs of anaphylaxis is not just about spreading information; it’s a life-saving measure. When an allergic reaction occurs, every second counts, and having people who can identify the symptoms can make a crucial difference in the outcome.
2. Recognizing Anaphylaxis:
- Understanding the signs and symptoms of anaphylaxis is the first step in effective intervention. Key indicators may include hives, swelling (especially around the face and throat), difficulty breathing, wheezing, a drop in blood pressure, nausea, vomiting, or loss of consciousness. Stress the importance of vigilance in recognizing these warning signs.
3. Administering Epinephrine Promptly:
- Epinephrine is the first-line treatment for anaphylaxis. It rapidly reverses the effects of the allergic reaction, buying valuable time until professional medical help arrives. Educate your close contacts on how to use an epinephrine auto-injector correctly, emphasizing the importance of administering it as soon as anaphylaxis is suspected.
4. Hands-On Training:
- Whenever possible, provide hands-on training sessions for family members and close friends. Allow them to practice with an epinephrine trainer device under your guidance or a healthcare professional’s supervision. This practical experience can boost their confidence and competence in an emergency.
5. Familiarize with Auto-Injectors:
- Different epinephrine auto-injectors may have variations in design and use instructions. Ensure that those close to you are familiar with the specific auto-injector you carry. Encourage them to read the device’s instructions and practice using it.
6. Highlight the Importance of Calling 911:
- Administering epinephrine is crucial, but it’s not a substitute for professional medical care. Teach your contacts that, after using the epinephrine auto-injector, they must call 911 or the local emergency number immediately. Anaphylaxis requires comprehensive medical evaluation and follow-up care.
7. Create an Emergency Plan:
- Develop an anaphylaxis emergency action plan that outlines the steps to take in case of an allergic reaction. Share this plan with your close contacts and keep a copy readily accessible in places like your home or workplace.
8. Encourage Open Communication:
- Foster an environment where your family and friends feel comfortable discussing your allergies and asking questions. Encourage them to seek clarification if they are unsure about anything related to anaphylaxis recognition or epinephrine administration.
9. Regular Updates and Refresher Training:
- Allergies and emergency response protocols can evolve. Schedule periodic updates and refresher training sessions to ensure that your close contacts remain knowledgeable and confident in their ability to respond effectively.
10. Express Gratitude: – Show appreciation to your family and friends for their willingness to learn and assist in managing your allergies. Their support and preparedness can alleviate anxiety and contribute to your safety and well-being.
In summary, teaching family members, friends, and close contacts about anaphylaxis recognition and the correct use of epinephrine is a vital aspect of allergy management. Their ability to respond swiftly and confidently during an allergic reaction can be a crucial factor in ensuring your safety and the successful management of anaphylaxis.
Looking for more insights? You’ll find them right here in our extended coverage: A qualitative study exploring parents’ experiences with epinephrine …
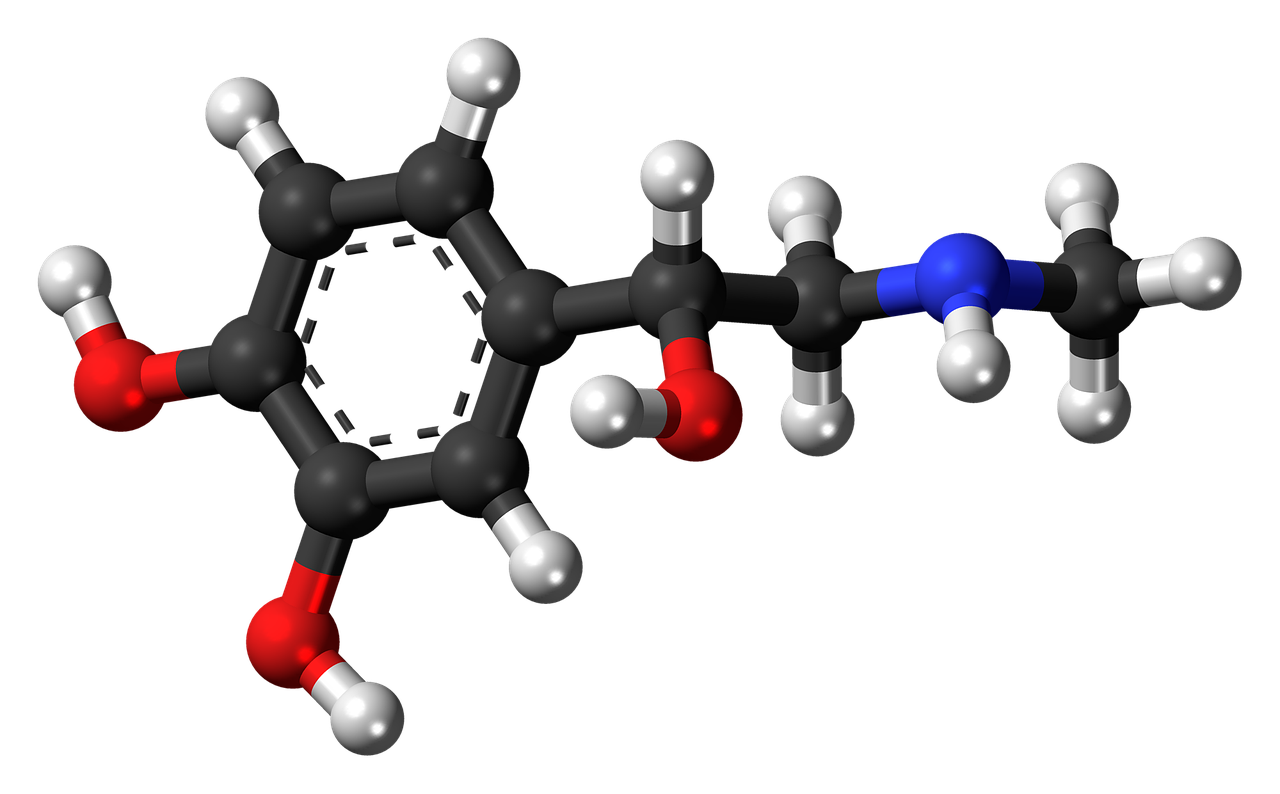
Conclusion
Anaphylaxis is a serious and potentially life-threatening allergic reaction that requires immediate attention and treatment. Epinephrine is a crucial tool in managing anaphylaxis and can be the difference between life and death. Understanding the causes and symptoms of anaphylaxis, as well as how to properly use epinephrine, is essential for anyone at risk of severe allergic reactions. By being prepared and taking preventative measures, individuals with allergies can lead safer and healthier lives. Remember, when in doubt, always seek medical help when anaphylaxis is suspected.
Anaphylaxis is a severe and potentially life-threatening allergic reaction that demands swift and decisive action. While it’s a distressing situation, knowledge and preparedness are your best allies in managing anaphylaxis effectively. Expanding on this crucial topic, let’s delve into the importance of understanding anaphylaxis, the role of epinephrine, and the broader implications for individuals at risk of severe allergic reactions:
Recognizing the Causes and Symptoms of Anaphylaxis: Anaphylaxis can be triggered by various allergens, including certain foods, insect stings, medications, and latex. It’s essential to be aware of your specific triggers, as well as the symptoms of anaphylaxis, which can include difficulty breathing, swelling of the face and throat, a rapid or weak pulse, nausea, and confusion. Understanding what may cause your allergic reactions and recognizing these symptoms promptly is the first step toward managing anaphylaxis effectively.
The Critical Role of Epinephrine: Epinephrine is often referred to as the “first-line treatment” for anaphylaxis, and for good reason. When administered promptly, it can reverse the dangerous effects of anaphylaxis by constricting blood vessels, increasing heart rate, relaxing airway muscles, and helping to alleviate symptoms such as low blood pressure, respiratory distress, and swelling. Always carry your prescribed epinephrine auto-injector and be familiar with its proper use.
Emergency Preparedness: Individuals at risk of anaphylaxis should have a well-thought-out anaphylaxis action plan in place. This plan should outline steps to take in the event of an allergic reaction, including the administration of epinephrine. Make sure family members, friends, and coworkers are aware of this plan and know how to assist you during an emergency. Consider wearing a medical alert bracelet to inform medical professionals of your allergies in case you are unable to communicate.
Preventative Measures: While it’s impossible to eliminate all potential allergen exposures, there are preventative measures you can take. Avoid your known allergens, read food labels carefully, inform restaurant staff about your allergies when dining out, and carry safe snacks or foods when traveling. When outdoors, take precautions against insect stings, such as wearing protective clothing and using insect repellent.
Regular Check-Ups: Schedule regular follow-up appointments with your allergist or immunologist to monitor your allergies and receive updated guidance on managing them. Allergies can change over time, and staying informed is crucial.
Support Networks: Consider joining support groups or online communities for individuals with severe allergies. Sharing experiences, strategies, and emotional support with others facing similar challenges can be immensely beneficial.
Advocate for Allergy Awareness: Advocate for allergy awareness and education within your community and workplace. Promoting understanding and preparedness can help ensure a safer environment for everyone, not just those with allergies.
In conclusion, anaphylaxis is a serious condition that demands vigilance, preparedness, and immediate action. Epinephrine is a life-saving tool, but knowing when and how to use it is equally important. By being proactive, understanding your allergies, and following preventative measures, you can lead a safer and healthier life while minimizing the risk of severe allergic reactions. Remember, in cases of doubt or suspicion of anaphylaxis, always seek immediate medical help. Being informed and prepared can make all the difference in managing this potentially life-threatening condition.
Looking for more insights? You’ll find them right here in our extended coverage: Safety of epinephrine for anaphylaxis in the emergency setting – PMC
More links
For additional details, consider exploring the related content available here Why Using Epinephrine for Allergic Reactions Works