Table of Contents
The practice of medicine is a delicate balance between the science of healing and the art of compassion. Medical professionals are entrusted with the well-being of their patients and face complex ethical dilemmas that require them to navigate a path between the rigors of science and the demands of human empathy. In this article, we explore the critical role of medical ethics in decision-making, emphasizing the importance of maintaining this delicate equilibrium.
nullFor a comprehensive look at this subject, we invite you to read more on this dedicated page: Foundations in Healthcare Ethics
The Ethical Imperative in Medicine
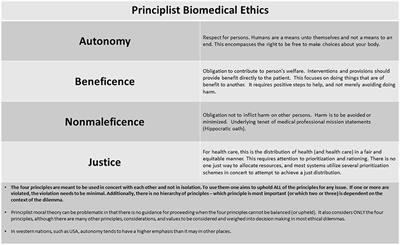
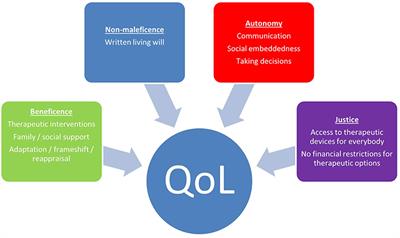
Medical ethics is the moral framework that guides healthcare professionals in making decisions that are in the best interest of their patients while upholding the principles of beneficence, non-maleficence, justice, and autonomy. These principles serve as the ethical compass in the often challenging terrain of healthcare.
Medical ethics is the moral framework that guides healthcare professionals in making decisions that are in the best interest of their patients while upholding the principles of beneficence, non-maleficence, justice, and autonomy. These principles serve as the ethical compass in the often challenging terrain of healthcare.
Balancing Act: Within the realm of medical ethics, healthcare providers face a delicate balancing act. Beneficence, or the duty to do good for the patient, drives them to provide the best care possible. Simultaneously, non-maleficence, or the obligation to do no harm, reminds them of the importance of minimizing risks and avoiding unnecessary suffering.
Justice and Fairness: The principle of justice underscores the importance of fairness and equity in healthcare decision-making. It challenges healthcare professionals to distribute resources and care equitably, considering the needs of all patients regardless of their background, socioeconomic status, or other factors. Achieving this balance can be complex, especially in resource-constrained environments.
Respecting Autonomy: Autonomy recognizes the patient’s right to make decisions about their own care, provided they have the capacity to do so. It’s about respecting the patient’s values, preferences, and choices, even when they may differ from the healthcare provider’s recommendations. Respecting autonomy can sometimes lead to challenging situations where patients make decisions that healthcare providers may personally disagree with.
Informed Consent: A critical application of autonomy is informed consent. It requires healthcare professionals to ensure that patients have all the necessary information to make decisions about their treatment. This process empowers patients to actively participate in their healthcare journey and aligns with the principles of autonomy and beneficence.
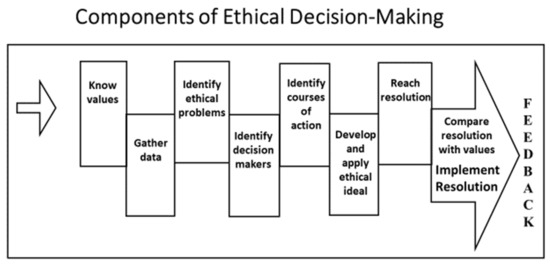
Ethical Dilemmas: Medical ethics often comes into sharp focus when healthcare providers encounter ethical dilemmas. These situations may involve end-of-life decisions, organ allocation, experimental treatments, or issues related to patient confidentiality. Navigating these dilemmas requires a deep understanding of ethical principles and a commitment to upholding patient welfare.
Continuous Ethical Reflection: Medical ethics isn’t a static set of rules but an ongoing process of ethical reflection and decision-making. As medical technology advances and society’s values evolve, healthcare professionals must adapt their ethical framework to address new challenges and dilemmas. This adaptability ensures that ethical principles remain relevant and applicable.
Patient-Centered Care: Ultimately, medical ethics plays a pivotal role in promoting patient-centered care. It guides healthcare providers in delivering care that not only aligns with medical standards but also respects the values and preferences of the individual patient. In this way, medical ethics helps create a healthcare system that is both clinically sound and ethically just.
In summary, medical ethics is the moral bedrock of healthcare, providing a framework that guides healthcare professionals in their pursuit of the best interests of their patients. It reminds them of the delicate balance between doing good and avoiding harm, promoting fairness, respecting autonomy, and navigating complex ethical dilemmas. Upholding these principles ensures that healthcare remains a noble and compassionate profession focused on improving the lives of individuals and communities.
For additional details, consider exploring the related content available here Beneficence and the professional’s moral imperative – PMC
Beneficence
The principle of beneficence underscores the obligation of healthcare professionals to act in the best interests of their patients, seeking to maximize benefits and well-being. It drives them to provide care that promotes health and healing.
The principle of beneficence, a cornerstone of ethical healthcare practice, not only emphasizes the duty of healthcare professionals to act in the best interests of their patients but also extends its reach far beyond the confines of medical treatment. This principle encapsulates a profound commitment to the holistic well-being of individuals, communities, and society at large.
At its core, beneficence compels healthcare professionals to go beyond the mere alleviation of symptoms and diseases. It beckons them to consider the broader context in which their patients exist, recognizing that health is not solely the absence of illness but the presence of physical, mental, and social well-being. In this regard, healthcare providers must adopt a patient-centered approach that encompasses not just the biological aspects of care but also the psychological, social, and cultural dimensions that influence health outcomes.
Moreover, the principle of beneficence places an ethical imperative on healthcare professionals to be advocates for health promotion and disease prevention. This means engaging in proactive efforts to educate patients and communities about healthier lifestyles, preventive measures, and the importance of early intervention. It calls for a shift from a reactive model of healthcare to a proactive one, where the focus is on maintaining wellness and preventing illness whenever possible.
In a broader societal context, beneficence compels healthcare professionals to address health disparities and systemic inequities. This principle underscores the obligation to advocate for policies and practices that ensure equitable access to quality healthcare for all, irrespective of race, ethnicity, socioeconomic status, or geographic location. In doing so, healthcare providers become catalysts for positive change in the healthcare system, aiming to eliminate the structural barriers that perpetuate health inequalities.
Furthermore, beneficence extends its reach to research and innovation in healthcare. Ethical research practices, guided by this principle, require the careful consideration of potential benefits and harms to participants and society. It necessitates rigorous ethical review processes to ensure that research is conducted with the utmost respect for the well-being and autonomy of those involved.
In essence, the principle of beneficence serves as a guiding light that compels healthcare professionals to act as not only healers but also advocates, educators, and champions of health and well-being for individuals and communities. It reminds us that healthcare is not just a profession; it is a profound commitment to the betterment of humanity, where the goal is not merely to treat illness but to nurture flourishing and thriving in every dimension of life.
Looking for more insights? You’ll find them right here in our extended coverage: Read the Belmont Report | HHS.gov
Non-Maleficence
Non-maleficence is the commitment to “do no harm.” Medical professionals must strive to minimize harm to their patients, ensuring that treatment decisions do not inadvertently cause suffering or exacerbate medical conditions.
Non-maleficence, the ethical principle rooted in the vow to “do no harm,” serves as a cornerstone of medical practice, guiding the actions and decisions of healthcare providers. This principle goes beyond a mere oath; it embodies the moral duty of medical professionals to safeguard the well-being and dignity of their patients in every aspect of care.
1. Treatment Efficacy: Non-maleficence compels medical professionals to thoroughly assess treatment options, not only considering their potential benefits but also their possible risks. This means carefully weighing the advantages of a procedure or medication against the potential harm it might cause. It emphasizes the importance of evidence-based medicine, where decisions are grounded in the best available knowledge to maximize benefits and minimize harm.
2. Informed Consent: Respecting non-maleficence requires that patients are fully informed about their treatment options, including potential risks and alternatives. Informed consent ensures that patients have the autonomy to make decisions in line with their values and preferences. It’s a testament to the respect for patient autonomy as a core principle of medical ethics.
3. Monitoring and Vigilance: Medical professionals must maintain a continuous vigilance throughout the course of treatment. Regular monitoring and assessment are crucial to detect any adverse effects promptly. Timely interventions can mitigate harm and ensure that the patient’s overall well-being is prioritized.
4. Ethical Dilemmas: In complex cases where the line between benefit and harm may be blurred, non-maleficence prompts ethical reflection and consultation. Medical ethics committees and consultations with colleagues can help navigate such challenging situations, ensuring that decisions are made with the utmost concern for the patient’s welfare.
5. Cultural Competence: Recognizing non-maleficence also extends to cultural competence. Medical professionals must be attuned to the diverse backgrounds, beliefs, and values of their patients. This cultural sensitivity helps prevent unintentional harm stemming from misunderstandings or insensitivity to cultural norms.
6. Advancements in Medicine: As medical science advances, the principle of non-maleficence takes on new dimensions. It demands that healthcare providers stay current with emerging treatments and technologies, ensuring that the benefits of progress are not overshadowed by unforeseen harms.
7. End-of-Life Care: Non-maleficence plays a pivotal role in end-of-life care decisions. Healthcare providers must weigh the potential suffering against the benefits of life-prolonging interventions, respecting the patient’s wishes and focusing on their comfort and dignity.
8. Ethical Challenges: Non-maleficence also addresses ethical challenges such as resource allocation and triage decisions during crises. It requires a commitment to fairness and equity, ensuring that scarce resources are distributed in a manner that minimizes harm to the greatest extent possible.
In essence, non-maleficence is a guiding light in the medical profession, illuminating the path toward ethical, compassionate, and patient-centered care. It reminds us that in every medical decision, the welfare of the patient must be paramount, and every effort must be made to prevent harm, uphold dignity, and alleviate suffering.
Don’t stop here; you can continue your exploration by following this link for more details: Patient Rights and Ethics – StatPearls – NCBI Bookshelf

Justice
The principle of justice demands fairness and equity in the allocation of healthcare resources and the treatment of patients. It underscores the importance of providing care without discrimination, regardless of factors such as race, ethnicity, or socioeconomic status.
nullTo delve further into this matter, we encourage you to check out the additional resources provided here: Moral Sentiment and the Sources of Moral Identity | Morality and the …
Autonomy
Autonomy recognizes the right of patients to make informed decisions about their healthcare. Medical professionals must respect their patients’ capacity to make choices and provide them with the information they need to do so.
Autonomy in healthcare is a fundamental principle that not only recognizes the right of patients to make informed decisions but also upholds their dignity and self-determination. It’s about much more than just respecting a patient’s capacity to make choices; it’s about empowering them to actively participate in their own care.
In a world where medical knowledge is vast and often complex, autonomy becomes a beacon of patient-centered care. It’s a commitment to transparency and communication. Medical professionals have a duty not only to provide patients with accurate and comprehensible information but also to engage in meaningful conversations that help patients understand their options, risks, and benefits.
Autonomy doesn’t end with the decision-making process; it extends to the implementation of those decisions. Medical professionals should work collaboratively with patients, ensuring that their choices are respected and integrated into their care plans. This collaborative approach fosters trust between patients and healthcare providers, leading to better adherence to treatment and improved health outcomes.
Moreover, autonomy recognizes the diversity of values and beliefs among patients. It respects that what might be the right choice for one patient may not be the same for another. It encompasses cultural sensitivity and the acknowledgment that individuals have different perspectives on health and well-being.
In essence, autonomy is the cornerstone of patient-centered healthcare. It’s a commitment to treating patients not as passive recipients of medical care but as active participants in their health journeys. It’s a reminder that every patient’s voice matters, and their choices should be honored and supported to the fullest extent possible.
Explore this link for a more extensive examination of the topic: Principles of Bioethics | UW Department of Bioethics & Humanities
Navigating Ethical Dilemmas
Medical professionals often face complex ethical dilemmas that require them to weigh competing interests and values. One common ethical challenge is the issue of informed consent. Ensuring that patients have a thorough understanding of their medical condition, treatment options, and potential risks is paramount. It requires clear and empathetic communication, allowing patients to make decisions aligned with their values and preferences.
Another ethical dilemma arises in end-of-life care decisions. Medical professionals must balance the pursuit of curative treatment with the patient’s desire for comfort and quality of life. These decisions can be emotionally charged and require sensitivity, empathy, and an understanding of the patient’s values and beliefs.
Don’t stop here; you can continue your exploration by following this link for more details: Ethics and Human Rights in Nursing | ANA
The Human Element in Decision-making
While medical ethics provides a structured framework for decision-making, it is the human element that breathes life into these principles. Compassion, empathy, and the ability to connect with patients on a personal level are essential aspects of ethical medical practice.
Medical professionals must not only understand the scientific aspects of a patient’s condition but also appreciate the emotional and psychological impact it has on the individual and their loved ones. By acknowledging the patient’s humanity, medical professionals can provide care that transcends the physical and touches the emotional and spiritual aspects of healing.
While medical ethics provides a structured framework for decision-making, it is the human element that breathes life into these principles. Compassion, empathy, and the ability to connect with patients on a personal level are not just desirable qualities but fundamental pillars of ethical medical practice.
In the practice of medicine, the patient is not merely a collection of symptoms, laboratory results, and medical history. They are a person with unique experiences, emotions, and vulnerabilities. Medical professionals must not only understand the scientific aspects of a patient’s condition but also appreciate the emotional and psychological impact it has on the individual and their loved ones.
Compassion and empathy play a pivotal role in establishing trust between healthcare providers and patients. When a patient senses that their medical team genuinely cares about their well-being, it can alleviate anxiety and foster a more collaborative relationship. Patients are more likely to openly share their concerns and adhere to treatment plans when they feel understood and valued as individuals.
Furthermore, by acknowledging the patient’s humanity, medical professionals can provide care that transcends the physical and touches the emotional and spiritual aspects of healing. This holistic approach recognizes that healing encompasses more than just addressing the immediate medical issue; it involves supporting patients through the emotional challenges, uncertainties, and fears that often accompany illness.
In essence, medical ethics forms the ethical foundation of healthcare, guiding professionals in making morally sound decisions. However, it is the infusion of compassion, empathy, and human connection that transforms these principles into meaningful actions, allowing medical professionals to provide care that not only heals the body but also uplifts the spirit and fosters a sense of healing and well-being in the patient. This fusion of ethics and humanity is what truly defines exemplary medical practice.
Don’t stop here; you can continue your exploration by following this link for more details: Jean Watson’s Theory of Human Caring | Redlands Community …
Balancing the Scales
Medical ethics and decision-making are a testament to the intricate interplay between science and compassion in the practice of medicine. While the science of medicine guides diagnosis and treatment, ethics ensures that these practices are grounded in the principles of humanity and moral duty.
Medical professionals must navigate this complex terrain with sensitivity, integrity, and a deep commitment to their patients’ well-being. By embracing both the scientific and compassionate dimensions of their profession, they strike a delicate yet essential balance that defines the art of medicine. In doing so, they honor their ethical obligations and uphold the sacred trust placed in them by their patients.
Explore this link for a more extensive examination of the topic: TIP 59: Improving Cultural Competence
More links
Explore this link for a more extensive examination of the topic: Principles of Clinical Ethics and Their Application to Practice – PMC
