Table of Contents
- Understanding Compassion Fatigue
- Continuous Exposure to Suffering
- Long Hours and High Workloads
- Lack of Resources
- High Expectations
- Recognizing Compassion Fatigue
- Emotional Exhaustion
- Depersonalization
- Reduced Empathy
- Physical Symptoms
- Promote Self-Care
- Mental Health Resources
- Peer Support Programs
- Staffing and Resource Improvements
- Education and Training
Medical professionals are among the most dedicated individuals, tirelessly working to save lives and provide compassionate care to those in need. However, the demanding nature of their jobs can often lead to a phenomenon known as “compassion fatigue.” This article explores what compassion fatigue is, its causes, signs, and most importantly, how to support and help our healthcare heroes combat this often-overlooked issue.
Medical professionals are among the most dedicated individuals, tirelessly working to save lives and provide compassionate care to those in need. However, the demanding nature of their jobs can often lead to a phenomenon known as “compassion fatigue.” This article explores what compassion fatigue is, its causes, signs, and most importantly, how to support and help our healthcare heroes combat this often-overlooked issue.
In the fast-paced and emotionally charged environment of healthcare, compassion fatigue can gradually wear down even the most resilient caregivers. It arises from the constant exposure to suffering, pain, and trauma, as well as the high-pressure decision-making and long hours that medical professionals face daily.
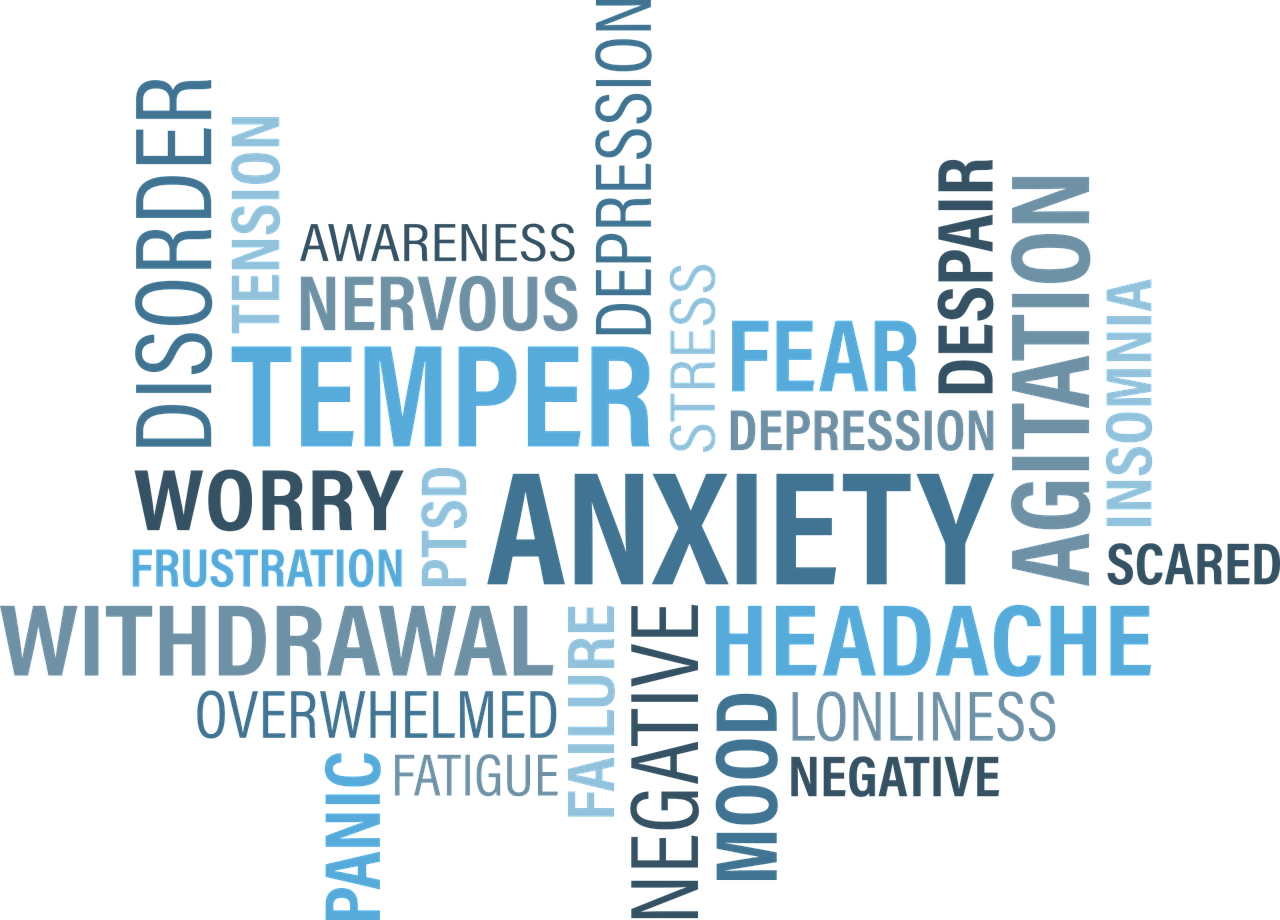
Recognizing the signs of compassion fatigue is crucial. It often manifests as emotional exhaustion, reduced empathy, increased irritability, and a decline in job satisfaction. Left unaddressed, it can lead to burnout, impacting not only the well-being of healthcare workers but also patient outcomes.
Supporting our healthcare heroes in combating compassion fatigue requires a multi-faceted approach. Institutions can implement wellness programs, offer regular mental health check-ins, and encourage a culture of open communication. Peer support networks and counseling services should be readily available. Additionally, it’s vital for healthcare professionals to prioritize self-care, set boundaries, and seek help when needed.
As a society, we owe it to these dedicated individuals to recognize the toll their work takes on their mental and emotional health and provide the necessary resources and understanding to help them continue their vital, life-saving work while maintaining their own well-being.
To expand your knowledge on this subject, make sure to read on at this location: Prioritizing the Mental Health and Well-Being of Healthcare Workers …
Understanding Compassion Fatigue
Compassion fatigue, also referred to as “secondary traumatic stress,” is a term used to describe the emotional and physical exhaustion experienced by individuals who care for others, especially in high-stress environments like healthcare. It’s not exclusive to doctors and nurses; it affects a wide range of medical professionals, including paramedics, radiologic technologists, and mental health workers.
Compassion fatigue, also referred to as “secondary traumatic stress,” is a term used to describe the emotional and physical exhaustion experienced by individuals who care for others, especially in high-stress environments like healthcare. It’s not exclusive to doctors and nurses; it affects a wide range of medical professionals, including paramedics, radiologic technologists, and mental health workers.
Widespread Impact: Compassion fatigue is not limited to the healthcare field alone; it can extend to professions like social work, emergency responders, and even educators. People in these roles often invest substantial emotional energy in helping others, making them susceptible to this phenomenon.
Signs and Symptoms: Recognizing compassion fatigue is crucial. Symptoms may include chronic fatigue, irritability, insomnia, decreased job satisfaction, and a sense of hopelessness. Left unaddressed, it can lead to burnout, affecting both the individual’s well-being and the quality of care they provide.
Prevention and Coping Strategies: Employers and individuals can take proactive steps to prevent compassion fatigue. This includes providing mental health resources, encouraging self-care, and promoting a supportive work environment. Practicing mindfulness, seeking counseling, and setting healthy boundaries are also effective coping strategies.
Patient Care Impact: When healthcare providers or professionals in other high-stress fields experience compassion fatigue, it can impact patient care. Reduced empathy and emotional exhaustion can lead to decreased quality of care and potential medical errors. Addressing compassion fatigue is, therefore, essential for the well-being of both caregivers and patients.
Training and Resilience Building: Incorporating resilience training and stress management techniques into professional development programs can help individuals in high-stress professions build emotional resilience and better cope with the challenges they face. This training can equip them with the tools to manage their emotional responses effectively.
Community Support: Community support networks can play a crucial role in helping professionals combat compassion fatigue. Peer support groups, employee assistance programs, and open dialogues about mental health can create a more compassionate and understanding work environment.
In conclusion, compassion fatigue is a pervasive issue that affects individuals across various high-stress professions. Recognizing its signs, implementing preventive measures, and providing support can help professionals in these fields maintain their well-being and continue to provide quality care to those they serve.
If you’d like to dive deeper into this subject, there’s more to discover on this page: Moving from compassion fatigue to compassion resilience Part 2 …

Continuous Exposure to Suffering
Healthcare workers witness human suffering and tragedy on a daily basis. The emotional toll of consistently encountering pain, illness, and death can accumulate over time.
Healthcare workers are the compassionate pillars of our society, tirelessly dedicating themselves to the well-being of others. Their daily routines bring them face to face with the profound aspects of human existence—both joy and sorrow. While they provide critical care and support, it’s essential to acknowledge the emotional toll that comes with their responsibilities.
The accumulation of emotional stress over time is a challenge that healthcare workers must navigate. Witnessing suffering, chronic illnesses, and even loss can be emotionally taxing. The empathy and compassion they extend to their patients often mean that they carry the weight of these experiences long after their shifts end.
It’s not uncommon for healthcare professionals to experience burnout, a state of emotional exhaustion and reduced personal accomplishment. The demands of their work can sometimes lead to feelings of helplessness and frustration, especially when they encounter barriers to providing the level of care they desire.
Furthermore, the COVID-19 pandemic has intensified these emotional challenges. Healthcare workers have faced unprecedented pressures, witnessing the devastating effects of the virus firsthand while dealing with their own personal fears and anxieties.
Acknowledging and addressing the emotional toll on healthcare workers is crucial for their well-being and the quality of care they provide. It’s essential to promote a culture of support within healthcare organizations, offering resources like counseling, peer support, and stress management programs. Encouraging self-care practices, such as exercise, mindfulness, and regular breaks, can also help mitigate the emotional strain.
Additionally, society as a whole must recognize and appreciate the sacrifices healthcare workers make daily. Expressing gratitude and offering emotional support can go a long way in helping them cope with the emotional challenges they face.
In conclusion, healthcare workers are the unsung heroes who witness the spectrum of human experience, from pain to recovery, joy to sorrow. Understanding and addressing the emotional toll they bear is essential to ensuring their well-being and sustaining their vital role in our healthcare system. By providing them with the support they need, we can help them continue to provide the compassionate care that defines their profession.
Should you desire more in-depth information, it’s available for your perusal on this page: Pandemic leads to compassion fatigue, burnout for health care …

Long Hours and High Workloads
The demanding schedules of medical professionals, often involving long shifts and overtime, leave little time for self-care, relaxation, and recovery.
nullFor a comprehensive look at this subject, we invite you to read more on this dedicated page: Prioritizing the Mental Health and Well-Being of Healthcare Workers …

Lack of Resources
In some healthcare settings, professionals may be working with limited resources, including insufficient staffing, inadequate equipment, or high patient-to-staff ratios, adding to their stress and frustration.
Working in healthcare can be immensely challenging, especially when professionals are tasked with delivering high-quality care in environments characterized by limited resources. These constraints, whether they involve insufficient staffing, outdated equipment, or overwhelming patient-to-staff ratios, can have far-reaching implications on the well-being of both healthcare workers and patients.
Insufficient staffing is a prevalent issue in many healthcare facilities. It places immense pressure on the existing workforce, often leading to burnout and compromised patient care. Overworked healthcare professionals may struggle to provide the attention and support patients need, which can result in lower quality outcomes and increased stress for everyone involved.
Inadequate equipment or outdated technology can hinder the efficiency and effectiveness of medical procedures. Healthcare professionals may find themselves having to make do with suboptimal tools, which can slow down diagnosis and treatment, potentially impacting patient outcomes and safety.
High patient-to-staff ratios exacerbate these challenges. When healthcare workers are stretched thin, they may struggle to meet the diverse needs of a larger patient population, making it difficult to provide the level of care they aspire to deliver. This can lead to frustration, burnout, and a sense of powerlessness among healthcare professionals.
Despite these challenges, healthcare professionals often show incredible resilience and dedication. They find innovative ways to optimize resources, provide compassionate care, and advocate for improvements in their work environments. However, addressing these resource limitations is essential to both alleviate the stress on healthcare workers and enhance the overall quality of healthcare for patients. It’s a shared responsibility that requires collaboration between healthcare organizations, policymakers, and society at large to ensure that our healthcare heroes have the support they need to thrive in their critical roles.
For additional details, consider exploring the related content available here Understanding the burnout experience: recent research and its …

High Expectations
Healthcare workers often place high expectations on themselves to provide the best possible care, which can lead to self-imposed pressure and guilt when they feel they haven’t done enough.
The dedication and commitment of healthcare workers are truly remarkable, but with that dedication often comes an internal struggle known as the “perfectionism trap.” Healthcare professionals are inherently driven by a genuine desire to provide the best possible care to their patients. This commitment to excellence is undoubtedly commendable, but it can also be a double-edged sword.
In the pursuit of perfection, healthcare workers may set impossibly high standards for themselves. They constantly seek to improve their skills, knowledge, and patient outcomes. While this relentless drive can lead to advancements in medical science and exceptional patient care, it can also manifest as self-imposed pressure.
These high expectations can take a toll on their mental and emotional well-being. When a medical professional perceives that they haven’t met their own lofty standards, it can lead to feelings of inadequacy and guilt. They may question their competence and dedication, even though they may be providing excellent care by objective standards.
Moreover, this self-imposed pressure can lead to burnout, a state of physical, mental, and emotional exhaustion that can have serious consequences for both the healthcare worker and their patients. Burnout can result in decreased job satisfaction, decreased quality of care, and increased rates of medical errors.
It’s essential to recognize that healthcare workers are human beings, not infallible superheroes. They will encounter challenges, make mistakes, and face situations where the outcome is beyond their control. Acknowledging these limitations is not a sign of weakness but a demonstration of self-awareness and humility.
To support healthcare professionals in navigating the perfectionism trap, institutions and colleagues can encourage a culture of self-compassion. This means fostering an environment where it’s okay to acknowledge one’s limitations, seek help when needed, and practice self-care without feelings of guilt. By doing so, we can help these dedicated individuals maintain their passion for healing, ensuring the best possible care for patients while safeguarding their own well-being. After all, healthcare workers who care for themselves can continue to care for others with even greater empathy and resilience.
To expand your knowledge on this subject, make sure to read on at this location: Caregiver Burnout: What It Is, Symptoms & Prevention
Recognizing Compassion Fatigue
Recognizing the signs of compassion fatigue is crucial for early intervention and support:
“Recognizing the signs of compassion fatigue is crucial for early intervention and support: In professions that require constant empathy and care for others, such as healthcare, social work, or emergency response, compassion fatigue can take a toll on the well-being of individuals. It’s more than just feeling tired; it’s a state of emotional exhaustion, reduced empathy, and a diminished sense of personal accomplishment.
Early detection of compassion fatigue is akin to identifying a storm on the horizon before it hits. When individuals, organizations, and support networks can spot the warning signs, they can take proactive steps to address and alleviate its impact.
This recognition empowers individuals to prioritize self-care, set healthy boundaries, and seek assistance when needed. Organizations can implement policies that promote a culture of well-being, offer resources for stress management, and provide opportunities for staff to debrief and share their experiences.
By shedding light on compassion fatigue and its symptoms, we create a more compassionate and resilient workforce, ultimately ensuring that those who dedicate themselves to caring for others can continue to do so with empathy and effectiveness.”
For additional details, consider exploring the related content available here Trauma, Compassion Fatigue, and Burnout in Nurses – PMC
Emotional Exhaustion
Feeling emotionally drained, numb, or detached from patients.
nullDon’t stop here; you can continue your exploration by following this link for more details: Compassion Fatigue, Secondary Traumatic Stress, and Vicarious …

Depersonalization
Developing a cynical or distant attitude towards patients and colleagues.
Developing a cynical or distant attitude towards patients and colleagues can have far-reaching consequences within the healthcare profession. This attitude, if left unchecked, can undermine the quality of care provided and erode the foundations of a supportive and compassionate work environment.
Diminished Patient Care: When healthcare professionals become cynical or distant, it can lead to a decline in the quality of patient care. Patients may perceive this attitude, which can result in reduced trust, reluctance to share critical information, and lower patient satisfaction.
Decreased Collaboration: A cynical or distant attitude can create barriers to effective collaboration among healthcare team members. Communication breakdowns and conflicts may arise, hindering the ability to provide coordinated care.
Mental and Emotional Toll: Maintaining a cynical or distant attitude can take a toll on healthcare professionals’ mental and emotional well-being. It can lead to burnout, compassion fatigue, and a sense of isolation.
Negative Work Environment: A pervasive negative attitude can permeate the work environment, contributing to a toxic workplace culture. This, in turn, can drive skilled professionals away from the field and make it challenging to attract and retain talent.
Ethical Concerns: A cynical attitude may erode ethical considerations in patient care. Healthcare professionals may become more inclined to prioritize personal interests over patient well-being, potentially leading to ethical lapses.
Reduced Job Satisfaction: Cynicism and distance can diminish job satisfaction, making healthcare professionals less engaged and passionate about their work. This, in turn, affects their commitment to continuous learning and improvement.
Legal and Regulatory Risks: A negative attitude may result in lapses in documentation, which can have legal and regulatory consequences. Neglecting proper record-keeping and communication can expose healthcare professionals and institutions to legal liability.
To counteract these negative consequences, healthcare organizations should prioritize promoting a culture of empathy, open communication, and continuous professional development. Encouraging self-awareness, stress management, and emotional resilience can help healthcare professionals navigate the challenges they face while maintaining a patient-centered, compassionate approach to their work. Ultimately, fostering a positive and supportive environment benefits both healthcare providers and the patients they serve.
For additional details, consider exploring the related content available here Understanding the burnout experience: recent research and its …

Reduced Empathy
Finding it increasingly difficult to empathize with patients’ suffering.
Finding it increasingly difficult to empathize with patients’ suffering can be a distressing experience for healthcare professionals, but it’s essential to recognize that this challenge often arises due to various factors within the healthcare system.
One contributing factor may be burnout, a pervasive issue in the healthcare industry. Healthcare providers often work long hours, handle high caseloads, and face emotionally demanding situations. Over time, this constant strain can lead to emotional exhaustion and reduced empathy. Addressing burnout through self-care, support systems, and organizational changes is crucial to help healthcare professionals maintain their compassion.
Another factor is desensitization, which can occur when healthcare workers repeatedly encounter traumatic or distressing situations. Initially, the emotional impact of witnessing suffering can be overwhelming, but as exposure becomes routine, individuals may develop a coping mechanism of detachment. To counter this, continuous training in empathy and compassion can be integrated into medical education and ongoing professional development.
The healthcare system’s bureaucratic and administrative burdens can also erode empathy. Spending excessive time on paperwork and navigating complex insurance processes can leave little energy for empathetic patient interactions. Streamlining administrative tasks and reducing paperwork can free up healthcare providers to focus on patient care.
Moreover, fostering a culture of empathy within healthcare organizations is essential. Encouraging open dialogue, peer support, and mental health resources can help professionals cope with the emotional toll of their work. Additionally, creating spaces for reflection and debriefing after challenging patient encounters can allow healthcare providers to process their emotions and regain empathy.
Ultimately, recognizing the difficulty in empathizing with patients’ suffering is the first step toward addressing this issue. By acknowledging the contributing factors and implementing strategies to support healthcare professionals, we can work toward preserving and enhancing empathy in healthcare, ultimately benefiting both patients and providers.
For a comprehensive look at this subject, we invite you to read more on this dedicated page: Examining the relationship between burnout and empathy in …

Physical Symptoms
Experiencing headaches, sleep disturbances, and other physical manifestations of stress.
Experiencing headaches, sleep disturbances, and other physical manifestations of stress can be incredibly challenging, often acting as warning signals from our bodies that something needs attention. These physical symptoms are more than mere inconveniences; they can have a profound impact on our overall well-being and daily life.
Headaches, for instance, can range from mild discomfort to debilitating pain, affecting our ability to concentrate, work, or even enjoy simple activities. Sleep disturbances, such as insomnia or restless nights, not only leave us fatigued but can also contribute to mood swings and a decreased ability to handle stress.
What’s crucial to understand is that these physical manifestations of stress are not isolated occurrences; they are interconnected with our mental and emotional state. Stress, when left unmanaged, can trigger a cascade of hormonal responses that can disrupt our body’s delicate balance. Chronic stress, in particular, has been linked to more serious health issues, including heart disease, digestive problems, and compromised immune function.
The good news is that recognizing these physical manifestations of stress provides an opportunity for self-care and proactive management. Taking steps to reduce stress through relaxation techniques, regular exercise, a balanced diet, and seeking support from friends, family, or professionals can make a significant difference. It’s essential to prioritize self-care and stress management not only for our physical health but also for our emotional and mental well-being.
In conclusion, experiencing physical symptoms of stress is a clear sign that our bodies are trying to communicate with us. By listening to these signals and taking steps to manage stress effectively, we can enhance our overall quality of life and ensure our physical, emotional, and mental health are in harmony.
Should you desire more in-depth information, it’s available for your perusal on this page: Compassion Fatigue among Healthcare, Emergency and …
Promote Self-Care
Encourage medical professionals to prioritize self-care and set boundaries. This includes taking regular breaks, getting adequate sleep, and engaging in activities that bring them joy.
nullExplore this link for a more extensive examination of the topic: Prioritizing the Mental Health and Well-Being of Healthcare Workers …

Mental Health Resources
Ensure access to mental health support services and resources. Normalizing seeking help for emotional well-being can reduce the stigma associated with asking for assistance.
Ensuring access to mental health support services and resources is a critical step in promoting overall well-being. However, it’s not just about providing these services; it’s also about fostering an environment where seeking help for emotional well-being is normalized and encouraged. Here are some key points to extend this idea:
Accessibility for All: To truly make a difference, mental health services must be accessible to everyone, regardless of their background, income, or location. This means increasing the availability of affordable or free mental health resources and ensuring they are geographically and culturally relevant.
Early Intervention: Normalizing the act of seeking help for emotional well-being encourages early intervention. When individuals feel comfortable discussing their mental health concerns openly, they are more likely to seek help at the first signs of distress, which can prevent issues from escalating.
Reducing Stigma: One of the most significant barriers to seeking mental health assistance is the stigma surrounding it. Efforts should be made to challenge stereotypes and misconceptions about mental health. Sharing personal stories of recovery and resilience can help break down these barriers.
Education and Awareness: Promoting mental health literacy is crucial. This includes educating people about common mental health conditions, their symptoms, and available treatments. When individuals understand that mental health issues are common and treatable, they are more likely to seek help without shame.
Supportive Workplaces and Communities: Employers and community leaders can play a pivotal role in normalizing mental health support. Workplace initiatives like Employee Assistance Programs (EAPs) and community campaigns can create environments where employees and community members feel safe discussing their mental health needs.
Peer Support Networks: Encouraging the development of peer support networks can be highly effective. When people see others who have gone through similar experiences and have benefited from seeking help, it can inspire them to do the same.
Cultural Competence: Recognize that different cultures may have unique perspectives on mental health. Efforts should be culturally sensitive, taking into account diverse beliefs and practices. This ensures that mental health support is inclusive and relevant to all communities.
Media and Entertainment: The media can contribute to both the stigma and destigmatization of mental health issues. Responsible and accurate portrayal of mental health in media can go a long way in normalizing discussions and encouraging help-seeking behavior.
Government and Policy: Government policies and funding play a significant role in mental health access and stigma reduction. Advocacy for mental health at the policy level can lead to increased resources and better mental health outcomes for communities.
In conclusion, ensuring access to mental health support services is essential, but it must go hand in hand with a concerted effort to change societal attitudes. By normalizing seeking help for emotional well-being and addressing the stigma surrounding mental health, we can create a more compassionate and supportive society that values the mental health and well-being of all its members.
If you’d like to dive deeper into this subject, there’s more to discover on this page: Caregiver Burnout: What It Is, Symptoms & Prevention

Peer Support Programs
Establish peer support groups or programs within healthcare facilities where medical workers can openly discuss their experiences and feelings with colleagues who understand the challenges they face.
Establishing peer support groups or programs within healthcare facilities is a proactive step towards nurturing the well-being of medical workers. In the high-pressure and emotionally demanding environment of healthcare, professionals often shoulder an immense burden. These support groups offer a safe space where they can openly discuss their experiences, emotions, and challenges with colleagues who intimately understand the unique trials they go through.
One of the remarkable aspects of these peer support programs is that they promote a culture of empathy and mutual aid among healthcare workers. These groups can foster a sense of camaraderie, providing validation to those who might otherwise feel isolated in their struggles. Sharing stories and coping strategies can be therapeutic in itself, helping individuals cope with the emotional toll of their work.
Furthermore, peer support can act as a preventive measure against burnout and mental health issues among healthcare workers. By addressing the stresses and traumas they encounter in a supportive environment, it becomes possible to mitigate the long-term impact on their mental well-being. In turn, this contributes to a more resilient and sustainable healthcare workforce.
It’s essential that these support programs are not only established but also actively encouraged and integrated into the healthcare system. This way, medical professionals can access the help they need without fear of stigma or repercussions. As we move forward, let’s recognize the value of these peer support initiatives in strengthening the healthcare workforce and, ultimately, improving patient care.
You can also read more about this here: Prioritizing the Mental Health and Well-Being of Healthcare Workers …

Staffing and Resource Improvements
Advocate for better staffing levels and resources within healthcare institutions to alleviate some of the workload pressures.
Advocating for better staffing levels and resources within healthcare institutions is not just a mere suggestion; it’s an imperative step toward improving the quality of patient care and the well-being of healthcare professionals. Here are several reasons why this advocacy is crucial:
1. Enhanced Patient Care: Adequate staffing ensures that healthcare providers can dedicate more time and attention to each patient. This leads to better diagnosis, treatment, and overall patient satisfaction. It’s the difference between rushed, impersonal care and compassionate, thorough treatment.
2. Reduced Burnout: Overworked healthcare professionals are at a high risk of burnout, which can result in physical and mental health issues. By increasing staffing levels, we can mitigate burnout, ensuring that healthcare workers remain healthy and motivated to provide the best care possible.
3. Safety: Inadequate staffing levels can compromise patient safety. When healthcare providers are stretched thin, they may make errors or overlook critical details. By advocating for better staffing, we can enhance patient safety and reduce the likelihood of medical errors.
4. Shorter Wait Times: Longer wait times for appointments, procedures, and emergency care can be frustrating and, in some cases, life-threatening. Improved staffing can help reduce these wait times, ensuring that patients receive timely care when they need it most.
5. Staff Well-Being: Adequate staffing not only benefits patients but also the well-being of healthcare professionals. It allows them to maintain a healthier work-life balance, reducing stress and improving their job satisfaction. This, in turn, can lead to better retention rates in the healthcare workforce.
6. Efficient Resource Utilization: Proper staffing also means optimizing the use of resources, from equipment to facilities. When healthcare institutions are adequately staffed, they can maximize the efficiency of their operations, reducing waste and costs.
7. Preparedness: Adequate staffing levels are critical during emergencies, whether it’s a pandemic, natural disaster, or a sudden influx of patients. Having a surplus of healthcare professionals ready to respond ensures that the healthcare system can adapt to unexpected challenges.
8. Attraction and Retention of Talent: Healthcare institutions that prioritize staffing are more likely to attract and retain top talent in the field. A robust workforce is essential for providing high-quality care and staying competitive in the healthcare industry.
In summary, advocating for improved staffing levels and resources in healthcare institutions is not just about easing the workload for healthcare professionals; it’s about enhancing patient care, promoting safety, and ensuring the overall well-being of both patients and those who dedicate their lives to caring for them. It’s a crucial step toward creating a healthier and more resilient healthcare system.
If you’d like to dive deeper into this subject, there’s more to discover on this page: Countering Compassion Fatigue: A Requisite Nursing Agenda | OJIN

Education and Training
Provide training on recognizing and coping with compassion fatigue as part of the professional development of medical workers.
nullTo expand your knowledge on this subject, make sure to read on at this location: Compassion Fatigue among Healthcare, Emergency and …

Compassion fatigue is a very real and serious issue affecting medical professionals who devote their lives to caring for others. Understanding its causes and recognizing the signs are crucial steps towards helping healthcare workers cope with the emotional toll of their profession. By offering support, resources, and fostering a culture of self-care and open communication, we can ensure that our medical heroes continue to provide the high-quality care that saves lives while safeguarding their own well-being. Compassion and empathy extend not only to patients but also to those who dedicate their lives to healing others.
Compassion fatigue is a very real and serious issue affecting medical professionals who devote their lives to caring for others. Understanding its causes and recognizing the signs are crucial steps towards helping healthcare workers cope with the emotional toll of their profession.
This phenomenon often arises from the constant exposure to suffering, trauma, and the relentless demands of medical practice. The relentless pressure to make critical decisions, long hours, and the inherent emotional intensity of patient care all contribute to the exhaustion that can lead to compassion fatigue.
Recognizing the signs of compassion fatigue is the first step in addressing this issue. It can manifest in various ways, such as emotional exhaustion, detachment from patients, increased cynicism, and a decrease in job satisfaction. Identifying these signs early allows for timely intervention and support, preventing further emotional and physical burnout.
Supporting healthcare professionals in their battle against compassion fatigue is a collective responsibility. Healthcare institutions can implement comprehensive wellness programs that provide access to mental health resources, peer support networks, and regular check-ins with mental health professionals. Fostering a culture of self-care and open communication is essential. This includes encouraging healthcare workers to set boundaries, take breaks, and seek help when needed without fear of judgment.
As a society, we owe it to these dedicated individuals to recognize the toll their work takes on their mental and emotional health. Our medical heroes save lives and provide essential care, often putting their own well-being on the line. Compassion and empathy should extend not only to patients but also to those who dedicate their lives to healing others. By offering unwavering support, resources, and understanding, we ensure that healthcare professionals can continue to provide the high-quality care that saves lives while safeguarding their own well-being. In doing so, we honor their dedication and commitment to the well-being of our communities.
Additionally, you can find further information on this topic by visiting this page: Compassion Fatigue – an overview | ScienceDirect Topics
More links
Don’t stop here; you can continue your exploration by following this link for more details: How to Cope with Compassion Fatigue in Healthcare | UCF Online
