Introduction
Statins, a class of medications known for their cholesterol-lowering properties, have been widely used to reduce the risk of cardiovascular diseases in adults. However, the use of statins in different age groups, particularly in pediatrics and geriatrics, raises unique considerations and challenges. In this article, we will explore the use of statins in these age groups, taking into account the benefits, potential risks, and special considerations that healthcare providers need to be aware of.
Statins, a class of medications renowned for their cholesterol-lowering properties, have played a pivotal role in reducing the risk of cardiovascular diseases in adults. However, as we delve into the realms of pediatrics and geriatrics, the use of statins presents unique considerations and challenges that warrant a closer examination. In this article, we embark on a journey through the nuanced landscape of statin therapy in these distinct age groups, carefully weighing the benefits, potential risks, and special considerations that healthcare providers must navigate.
Pediatrics: Nurturing Healthy Foundations
In the realm of pediatrics, the use of statins represents a response to the growing concern of early-onset hyperlipidemia and its potential long-term consequences. Statins can be considered when lifestyle modifications alone prove insufficient in managing cholesterol levels in children and adolescents. However, prescribing statins to this age group demands a delicate balance between reaping the benefits of cholesterol reduction and mitigating potential risks.
The benefits of statin therapy in pediatrics are grounded in the prevention of early atherosclerotic changes, which can carry through to adulthood. Nevertheless, special considerations abound, including the need for rigorous monitoring, careful selection of appropriate candidates, and ongoing communication with young patients and their families.
Geriatrics: Navigating Complex Terrain
Conversely, the geriatric population poses its own set of challenges and opportunities in statin therapy. As individuals age, the risk of cardiovascular diseases increases, making statins a valuable tool in reducing this risk. Yet, the elderly often contend with multiple comorbidities, an array of medications, and age-related changes in drug metabolism, all of which necessitate a nuanced approach.
Benefits in the geriatric population include the potential to enhance cardiovascular health and prolong an active, independent lifestyle. However, healthcare providers must be vigilant in assessing the risk of drug interactions, monitoring for side effects, and adapting treatment plans to suit the unique needs of older individuals.
A Journey of Considerations
In traversing the landscape of statin use across age groups, it becomes evident that the benefits extend far beyond cholesterol reduction. Statins hold the promise of preserving health, preventing disease, and improving the quality of life. Nevertheless, they must be administered with care, and decisions should be rooted in a thorough understanding of the individual patient’s needs, medical history, and goals.
As we embark on this journey through the use of statins in pediatrics and geriatrics, we shed light on the delicate balance that healthcare providers must strike. The decision to prescribe, monitor, or adjust statin therapy requires a deep appreciation for the unique considerations of each age group. Ultimately, it is through such understanding and meticulous care that we can harness the full potential of statins while safeguarding the well-being of those we seek to benefit.
If you’d like to dive deeper into this subject, there’s more to discover on this page: 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC …
The use of statins in pediatric populations has gained attention in recent years, primarily due to the increasing prevalence of childhood obesity and its associated health risks, including high cholesterol levels. Here are some key considerations when it comes to statin use in children:
The growing concern surrounding the use of statins in pediatric populations is closely linked to the rising rates of childhood obesity. Childhood obesity has reached alarming proportions in many parts of the world and is a significant public health issue. It is often accompanied by a range of health problems, including elevated cholesterol levels, which can increase the risk of early cardiovascular disease.
1. The Pediatric Obesity Epidemic:
- The global increase in childhood obesity has raised concerns about related health conditions, such as dyslipidemia, which refers to abnormal lipid (fat) levels in the blood.
- Dyslipidemia, particularly high levels of LDL cholesterol, can accelerate the development of atherosclerosis (hardening and narrowing of the arteries) even in childhood, setting the stage for future cardiovascular issues.
2. Familial Hypercholesterolemia (FH):
- One of the primary reasons for considering statin therapy in children is the presence of familial hypercholesterolemia (FH), an inherited genetic condition characterized by extremely high cholesterol levels.
- Children with FH are at a substantially increased risk of early cardiovascular events, making early intervention with statins a potentially life-saving measure.
3. Lifestyle Modifications as the First Line of Defense:
- Before turning to statin therapy, healthcare providers emphasize lifestyle modifications as the initial approach to managing high cholesterol in children.
- Dietary changes, increased physical activity, and weight management are critical components of addressing cholesterol issues in pediatric patients.
4. Statin Therapy for High-Risk Cases:
- Statin therapy in children is typically reserved for those with severe FH or extremely high cholesterol levels that do not respond adequately to lifestyle changes.
- The decision to initiate statin treatment is made on a case-by-case basis and involves careful evaluation of the child’s cardiovascular risk.
5. Ongoing Research and Monitoring:
- Given the unique considerations of pediatric statin use, ongoing research is essential to assess the long-term safety and effectiveness of these medications in children.
- Monitoring for potential side effects, such as muscle pain and liver enzyme elevation, is a critical part of pediatric statin therapy.
6. Multidisciplinary Care:
- The management of high cholesterol in children often requires a multidisciplinary approach that involves pediatricians, pediatric cardiologists, and registered dietitians.
- Collaborative care ensures that treatment decisions align with the child’s overall health and well-being.
7. Parent and Caregiver Involvement:
- Engaging parents and caregivers is crucial in pediatric cholesterol management. They play a vital role in implementing lifestyle changes and ensuring medication adherence.
- Parental support and understanding can significantly impact a child’s ability to manage cholesterol effectively.
In conclusion, the consideration of statin therapy in pediatric populations is driven by the increasing prevalence of childhood obesity and its associated health risks. While lifestyle modifications remain the cornerstone of cholesterol management in children, statins are reserved for high-risk cases, particularly those with familial hypercholesterolemia. The decision to initiate statin therapy is a careful one, involving healthcare providers, caregivers, and the child in question, with a focus on long-term cardiovascular health and well-being. Ongoing research and monitoring will continue to shape our understanding of statin use in pediatrics.
To expand your knowledge on this subject, make sure to read on at this location: Statin Therapy in Older Adults for Primary Prevention of …

Familial hypercholesterolemia (a genetic condition causing high cholesterol) is the primary indication for statin therapy in children.
Lifestyle modifications, including dietary changes and increased physical activity, are typically the first line of treatment for children with elevated cholesterol levels.
Familial hypercholesterolemia (FH), a genetic condition characterized by abnormally high cholesterol levels, can affect individuals from a young age, including children. For these young patients, statin therapy serves as a crucial treatment strategy. However, it’s important to note that the decision to initiate statin therapy in children is carefully considered and typically reserved for those with severe FH or those at significant risk of early cardiovascular disease.
In many cases, lifestyle modifications are the initial approach to managing elevated cholesterol levels in children. These modifications include dietary changes aimed at reducing saturated and trans fats, as well as an emphasis on consuming heart-healthy foods like fruits, vegetables, whole grains, and lean proteins. Portion control and limiting sugary beverages also play a role in improving overall diet quality.
Physical activity is another cornerstone of pediatric cholesterol management. Encouraging children to engage in regular physical activity not only helps with weight management but also positively impacts cholesterol levels. Active play, sports, and other age-appropriate activities not only contribute to better cardiovascular health but also foster lifelong habits of physical fitness.
However, in cases where lifestyle modifications alone are insufficient to manage cholesterol levels in children with FH, statin therapy may be considered. Statins work by reducing the production of cholesterol in the liver and increasing the liver’s ability to remove LDL cholesterol from the bloodstream. For children with severe FH, early initiation of statin therapy can be a critical step in reducing the risk of premature heart disease.
It’s crucial to emphasize that the decision to use statins in children is a complex one and is typically made in consultation with a pediatric cardiologist or lipid specialist. The benefits of statin therapy must be weighed against potential risks and side effects, and ongoing monitoring is essential to ensure the child’s safety and effectiveness of treatment.
In summary, while lifestyle modifications are the first line of treatment for children with elevated cholesterol levels, familial hypercholesterolemia presents a unique situation where statin therapy may be necessary. The key is to provide a comprehensive approach to pediatric heart health that combines dietary improvements, physical activity, and, when appropriate, medical intervention to safeguard the well-being of children at risk of cardiovascular disease.
Don’t stop here; you can continue your exploration by following this link for more details: 2019 ACC/AHA Guideline on the Primary Prevention of …

Statins can effectively lower cholesterol levels in pediatric patients, reducing their risk of early cardiovascular events.
However, the long-term safety of statins in children is a subject of ongoing research and monitoring.
Potential side effects, such as muscle pain and liver enzyme elevations, need to be carefully monitored.
The use of statins in pediatric patients marks a significant stride in the realm of preventive medicine. These medications have demonstrated their effectiveness in lowering cholesterol levels among young individuals, thereby mitigating the risk of early cardiovascular events. However, as we tread this path, it’s crucial to acknowledge that the long-term safety of statins in children remains an ongoing subject of research and vigilant monitoring.
1. Early Intervention: The decision to prescribe statins to pediatric patients is typically guided by a careful assessment of their individual risk factors and cholesterol levels. For children with familial hypercholesterolemia or other underlying conditions predisposing them to elevated cholesterol, statins can be a crucial tool in early intervention. By starting treatment during childhood, healthcare providers aim to establish a solid foundation for heart health, potentially preventing the progression of cardiovascular disease into adulthood.
2. Safety in Focus: While the benefits of statins in pediatric patients are promising, it’s essential to maintain a vigilant eye on their safety profile. Potential side effects, such as muscle pain (myalgia) and elevations in liver enzymes, are areas of particular concern. Close monitoring is imperative to detect and address these side effects promptly. The risk of adverse events is generally considered low in children, but individual responses can vary, emphasizing the importance of personalized care.
3. Multidisciplinary Approach: The decision to prescribe statins to children is not taken lightly. It often involves a multidisciplinary team of healthcare professionals, including pediatricians, cardiologists, and dietitians. This collaborative approach ensures that the benefits and risks are thoroughly evaluated, and the treatment plan is tailored to the child’s unique needs and circumstances.
4. Lifelong Commitment to Health: When statins are prescribed to pediatric patients, it signifies a commitment to long-term health and well-being. These medications are not a short-term fix but a part of a comprehensive strategy to reduce cardiovascular risk over a lifetime. Regular check-ups, blood tests, and ongoing communication between healthcare providers and families are essential components of this commitment.
5. Informed Decision-Making: Involving parents or guardians in the decision-making process is crucial. It’s essential for families to be well-informed about the rationale behind statin therapy, potential side effects, and the expected benefits. Open and transparent communication between healthcare providers and families helps ensure that everyone is on the same page and can actively participate in managing the child’s health.
In conclusion, the use of statins in pediatric patients represents a proactive approach to addressing elevated cholesterol levels and reducing the risk of early cardiovascular events. While the potential benefits are promising, ongoing research and vigilant monitoring are necessary to assess the long-term safety and efficacy of statins in children. With a multidisciplinary approach, informed decision-making, and a commitment to lifelong health, we can work toward ensuring that statin therapy for pediatric patients remains a well-informed and carefully managed strategy for promoting heart health from an early age.
Additionally, you can find further information on this topic by visiting this page: 2019 ACC/AHA Guideline on the Primary Prevention of …

Pediatric statin therapy requires a multidisciplinary approach involving pediatricians, pediatric cardiologists, and dietitians.
Close monitoring and ongoing evaluation are essential to ensure that the benefits of statin therapy outweigh any potential risks.
Pediatric statin therapy represents a specialized area of care, demanding a collaborative and multidisciplinary approach. The well-being of young patients is at the forefront, and as such, a dedicated team comprising pediatricians, pediatric cardiologists, and dietitians comes together to provide comprehensive and individualized care.
Pediatricians: These healthcare professionals serve as the primary point of contact for families and patients, guiding them through the complexities of statin therapy. Pediatricians are responsible for conducting thorough assessments, considering family medical histories, and diagnosing conditions that necessitate statin treatment. They play a crucial role in communicating with parents and caregivers, explaining the benefits, potential risks, and expected outcomes of statin therapy in a way that is understandable and reassuring.
Pediatric Cardiologists: Pediatric cardiologists bring their specialized expertise to the table. They possess a deep understanding of heart health in children, allowing them to assess the cardiovascular condition in detail. These specialists work in tandem with pediatricians to determine the most appropriate treatment plan, closely monitor the child’s progress, and make necessary adjustments to medication regimens as needed. Their insights are invaluable in ensuring the safety and efficacy of statin therapy in young patients.
Dietitians: Proper nutrition plays a pivotal role in pediatric statin therapy. Dietitians collaborate with families and patients to develop tailored dietary plans that complement the medication regimen. They focus on heart-healthy eating habits, emphasizing the importance of balanced diets rich in whole grains, fruits, vegetables, and lean proteins. Dietitians also educate families on the significance of reducing saturated and trans fats and moderating cholesterol intake through food choices. Their guidance empowers families to make nutritious choices that enhance the overall effectiveness of statin therapy.
Close Monitoring: The careful and ongoing monitoring of pediatric patients receiving statin therapy is a paramount consideration. Regular check-ups and follow-up appointments are scheduled to assess the child’s response to treatment. Through blood tests, the healthcare team can closely monitor cholesterol levels, liver function, and any potential side effects, ensuring that the benefits of statin therapy are maximized while any risks are promptly addressed.
Ongoing Evaluation: Pediatric statin therapy is not static; it evolves as the child grows and responds to treatment. Regular evaluations help assess the need for adjustments in medication dosages or treatment plans. The multidisciplinary team stays vigilant, ensuring that the child’s cardiovascular health remains a top priority.
In the realm of pediatric statin therapy, collaboration and vigilance are key. It’s a delicate balance between managing cholesterol levels effectively and safeguarding the well-being of young patients. The multidisciplinary approach, which leverages the expertise of pediatricians, pediatric cardiologists, and dietitians, helps strike that balance. It assures parents and caregivers that their child’s heart health is being managed with the utmost care, consideration, and expertise, ultimately laying the foundation for a healthier and more vibrant future.
For additional details, consider exploring the related content available here Standards of Medical Care in Diabetes—2022 Abridged for Primary …
In the elderly population, statin use presents a different set of considerations:
In the elderly population, statin use presents a different set of considerations that warrant careful evaluation and personalized decision-making. Age-related changes in metabolism, potential interactions with other medications commonly used by older adults, and the presence of multiple chronic conditions can all influence the appropriateness and safety of statin therapy in this demographic.
One crucial factor to weigh is the potential benefit of statins in older individuals. While statins are proven to reduce the risk of cardiovascular events, the absolute risk reduction may vary among elderly patients, especially if they have limited life expectancy or are dealing with multiple comorbidities. Healthcare providers must assess whether the potential cardiovascular benefits outweigh the risks and potential side effects in each unique case.
Additionally, the risk of adverse effects from statins, such as muscle-related symptoms or liver abnormalities, may be heightened in older adults due to age-related changes in drug metabolism and decreased organ function. Hence, regular monitoring and close communication with healthcare providers are essential to ensure the safe and effective use of statins in older individuals.
Ultimately, the decision to prescribe statins to the elderly should be a collaborative one, involving thorough discussions between healthcare providers and patients or their caregivers. This patient-centered approach takes into account individual health status, goals of care, and the potential for shared decision-making to arrive at the most appropriate treatment plan. In this way, statin therapy in the elderly can be tailored to optimize both cardiovascular health and overall well-being.
To expand your knowledge on this subject, make sure to read on at this location: Risks of Statin Therapy in Older Adults | Cardiology | JAMA Internal …

Statins have demonstrated significant benefits in reducing the risk of cardiovascular events in older adults.
However, the potential for side effects and drug interactions increases with age, necessitating a careful benefit-risk assessment.
The efficacy of statins in lowering the risk of cardiovascular events among older adults is a compelling and well-documented finding. As individuals age, their susceptibility to heart-related issues often rises, making the role of statins in promoting cardiovascular health even more critical. These medications can help mitigate the potential consequences of conditions like high cholesterol and atherosclerosis, offering a lifeline to many seniors.
Yet, it’s crucial to acknowledge that as age advances, so does the complexity of healthcare. Statins, like any medication, come with the possibility of side effects and interactions, and these risks tend to increase in older populations. Therefore, it becomes imperative for healthcare providers to conduct a meticulous benefit-risk assessment before initiating statin therapy in older adults.
This assessment involves a thorough evaluation of an individual’s overall health, medical history, and potential risk factors for side effects. Common side effects of statins, such as muscle pain or liver abnormalities, may be more prevalent or severe in older adults due to age-related physiological changes or the presence of other chronic conditions.
Additionally, the potential for drug interactions must not be overlooked, as older adults often take multiple medications to manage various health concerns. Statins can interact with other drugs, affecting their efficacy or safety. A comprehensive review of an individual’s medication list is essential to identify and mitigate potential interactions.
Despite these considerations, the benefits of statin therapy in older adults should not be underestimated. The protection they offer against heart attacks, strokes, and other cardiovascular events can be profound, potentially extending both lifespan and overall quality of life. However, the decision to prescribe statins to older adults should always be an informed and individualized one, taking into account the unique circumstances and health status of each patient.
In conclusion, while statins represent a powerful tool in reducing cardiovascular risk among older adults, a judicious approach to their use is paramount. A careful balance between the benefits and risks must be struck, with healthcare providers playing a vital role in tailoring statin therapy to meet the specific needs and conditions of their older patients. Through thoughtful assessment and personalized care, the potential benefits of statins can be maximized while minimizing the associated risks, ensuring that seniors can enjoy heart-healthy and fulfilling lives.
To expand your knowledge on this subject, make sure to read on at this location: Recommendation: Statin Use for the Primary Prevention of …
Treatment decisions regarding statins in geriatrics should be highly individualized.
Factors such as overall health, life expectancy, and the presence of multiple chronic conditions should be taken into account.
In the realm of geriatric care, making informed treatment decisions about statins is an intricate and highly personalized process. Recognizing the uniqueness of each elderly patient’s situation is paramount, and several key factors must be carefully weighed and considered.
Overall Health: The general health status of an elderly individual plays a pivotal role in determining the appropriateness of statin therapy. While some older adults may be in robust health with minimal age-related complications, others may face multiple chronic conditions or physical limitations. The impact of statin therapy on overall well-being should be assessed, considering the individual’s capacity to tolerate potential side effects or interactions with other medications.
Life Expectancy: Life expectancy is a crucial factor in the decision-making process. For individuals with a limited life expectancy due to advanced age or severe illness, the potential long-term benefits of statin therapy may be outweighed by the burden of ongoing treatment and the possibility of adverse effects. Conversations between healthcare providers and patients or their families should encompass the patient’s goals and values, guiding the decision in alignment with their desires for quality of life in their remaining years.
Chronic Conditions: The presence of multiple chronic conditions often characterizes geriatric patients. Diabetes, hypertension, heart disease, and kidney disease are just a few examples. In such cases, a thorough assessment of the interplay between these conditions and the potential benefits or risks of statin therapy is essential. It may be necessary to prioritize certain conditions over others or to tailor statin treatment to minimize adverse effects.
Functional Status: The functional status of an older adult, including their ability to perform daily activities independently, is a crucial consideration. Statin therapy should not unduly compromise an individual’s quality of life or functional independence. A thorough evaluation of the patient’s mobility, cognitive function, and self-care abilities is essential in determining the appropriateness of statin therapy.
Patient Preferences: In shared decision-making, the preferences and values of the elderly patient should take center stage. Their input regarding their health goals, treatment preferences, and concerns about statin therapy should be actively sought and respected. In some cases, patients may prioritize symptom management or maintaining independence over cholesterol control, influencing the treatment plan accordingly.
In essence, the decision to initiate or continue statin therapy in geriatrics is multifaceted and should be rooted in a comprehensive assessment of the individual’s health, circumstances, and preferences. Embracing a patient-centered approach ensures that the chosen course of action aligns with the older adult’s unique needs and goals, fostering a harmonious balance between health maintenance and quality of life as they age gracefully.
For additional details, consider exploring the related content available here Standards of Medical Care in Diabetes—2022 Abridged for Primary …
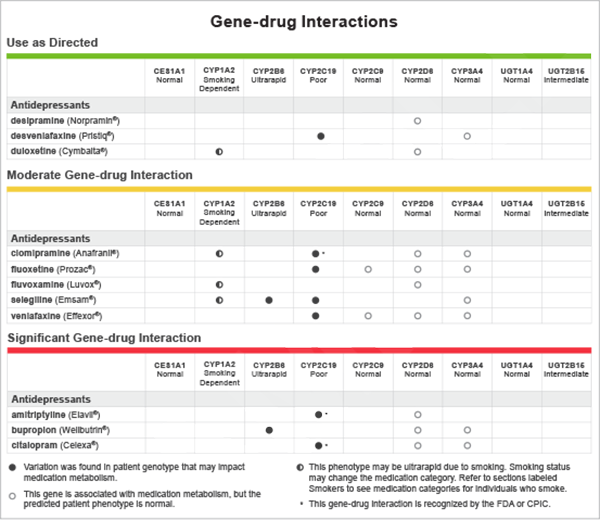
Older adults often take multiple medications for various health conditions, increasing the risk of drug interactions.
Healthcare providers must carefully consider potential interactions between statins and other medications, especially those metabolized through the same pathways.
Older adults often take multiple medications for various health conditions, increasing the risk of drug interactions—a phenomenon sometimes referred to as “polypharmacy.” Managing polypharmacy is a critical aspect of geriatric care, and when it comes to statins, healthcare providers must be especially diligent. Here’s why:
Complex Medication Regimens: Older adults often have complex medication regimens, encompassing drugs for heart health, blood pressure control, diabetes management, and more. Adding statins to the mix requires a thorough review of potential interactions to ensure the safety and efficacy of the overall treatment plan.
Metabolic Pathways: Statins are metabolized primarily in the liver, as are many other medications. When multiple drugs compete for the same metabolic pathways, it can lead to altered drug levels in the bloodstream. This can potentially result in reduced effectiveness or increased risk of side effects.
Blood-Thinning Medications: For older adults at risk of heart disease, it’s common to be on both statins and blood-thinning medications like aspirin or anticoagulants. Managing the delicate balance between preventing clotting and maintaining cholesterol levels requires close monitoring and careful dosing adjustments.
Comprehensive Assessment: Healthcare providers must conduct a comprehensive assessment of an older adult’s medical history, current health conditions, and all medications being taken. This assessment includes over-the-counter drugs, supplements, and herbal remedies, as they can also interact with statins.
Personalized Medicine: Recognizing that individual responses to medications can vary widely, a personalized medicine approach is crucial for older adults. Healthcare providers should tailor treatment plans, considering each patient’s unique health profile and risk factors.
Regular Monitoring: Close monitoring is essential when older adults are prescribed statins in conjunction with other medications. Regular check-ups and blood tests help detect any adverse effects or interactions early, allowing for timely adjustments.
Communication: Effective communication between healthcare providers, patients, and caregivers is vital. Patients should be encouraged to report any unusual symptoms or side effects promptly, and caregivers can play a vital role in ensuring medication adherence and monitoring for potential issues.
Deprescribing When Appropriate: In some cases, deprescribing—gradually reducing or discontinuing medications that may no longer be necessary or pose risks—can be a valid strategy. Healthcare providers should regularly assess whether all prescribed medications remain essential.
Pharmacist Involvement: Pharmacists are valuable resources in managing polypharmacy. They can conduct medication reviews, identify potential interactions, and collaborate with healthcare providers to optimize medication regimens.
In essence, the management of statin therapy in older adults involves a delicate balancing act, one that requires a deep understanding of both the patient’s medical history and the pharmacological properties of the medications involved. The goal is to maximize the benefits of statins while minimizing the risks associated with drug interactions, ensuring that older adults receive safe and effective care for their cardiovascular health.
Should you desire more in-depth information, it’s available for your perusal on this page: 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC …
Statin-associated muscle symptoms can be more common in older adults.
Healthcare providers should be vigilant in monitoring for muscle pain and weakness, which may require dose adjustments or discontinuation of statin therapy.
Statin-associated muscle symptoms, often referred to as SAMS, tend to be more prevalent in older adults due to age-related changes in muscle function and metabolism. Therefore, it’s crucial for healthcare providers to maintain a heightened sense of awareness when prescribing statins to this demographic.
Older adults are often prescribed statins as a preventive measure against heart disease and stroke, given their increased susceptibility to these conditions. However, their age can also make them more vulnerable to SAMS. Muscle pain and weakness can be particularly concerning in older individuals because they can limit mobility and affect overall quality of life.
Regular and thorough monitoring is essential when older adults are on statin therapy. Healthcare providers should actively inquire about any muscle-related symptoms during check-ups and encourage patients to report any discomfort promptly. This open communication allows for the early detection of SAMS, which is crucial for timely intervention.
If muscle symptoms do arise, healthcare providers have several options. They may consider adjusting the statin dosage, switching to a different type of statin, or even temporarily discontinuing statin therapy to alleviate the symptoms. The goal is always to find the right balance between cholesterol management and preserving muscle function.
Additionally, healthcare providers should take a comprehensive approach to care for older adults on statins. This includes addressing other factors that may contribute to muscle symptoms, such as concomitant medications and underlying medical conditions. Adjusting other medications or managing comorbidities can sometimes help mitigate SAMS.
Ultimately, the decision regarding statin therapy in older adults should be made on an individual basis, weighing the potential cardiovascular benefits against the risk of muscle-related side effects. It’s a nuanced process that requires careful consideration, regular monitoring, and open communication between healthcare providers and their older patients to ensure the best possible outcomes for heart health while preserving overall well-being.
Don’t stop here; you can continue your exploration by following this link for more details: Statin Medications – StatPearls – NCBI Bookshelf

In both pediatrics and geriatrics, the use of statins necessitates a tailored, patient-centered approach. For pediatric patients, statins are reserved for those with specific genetic conditions or severe hypercholesterolemia, with lifestyle modifications as the initial strategy. In geriatric patients, the decision to prescribe statins should consider the potential benefits, risks, and the complexity of managing multiple health conditions and medications.
Regardless of age group, communication between patients and healthcare providers is crucial. Informed decision-making, careful monitoring, and a focus on individual patient needs are essential components of statin therapy in pediatrics and geriatrics alike.
You can also read more about this here: Standards of Medical Care in Diabetes—2022 Abridged for Primary …
More links
Don’t stop here; you can continue your exploration by following this link for more details: Management of Dyslipidemia in the Elderly – Endotext – NCBI …
