Introduction
Statins have been a cornerstone in the management of cholesterol levels and the prevention of cardiovascular disease in both men and women. However, specific considerations arise when discussing statin use in the context of women’s health. In this article, we will explore the implications of statin therapy during pregnancy and menopause, shedding light on the factors that healthcare providers and women themselves should consider.
Statins have unquestionably played a crucial role in the management of cholesterol levels and the prevention of cardiovascular disease in both men and women. However, it is essential to recognize that specific considerations arise when discussing statin use in the context of women’s health. In this article, we will delve deeper into the implications of statin therapy during pregnancy and menopause, shedding light on the factors that healthcare providers and women themselves should consider.
Statins and Pregnancy: Balancing Risks and Benefits
Pregnancy is a unique phase in a woman’s life where the health of both the mother and the developing fetus is of paramount importance. Statin use during pregnancy is generally discouraged due to potential concerns about fetal development. While there is limited research on the safety of statins during pregnancy, animal studies have raised some questions about their potential to cause birth defects.
Therefore, it is crucial for women who are planning to become pregnant or who are already pregnant to discuss statin use with their healthcare provider. In cases where statins are deemed necessary to manage extremely high cholesterol levels in pregnant women, the decision to use these medications must be made cautiously, weighing the potential benefits against the possible risks to the fetus. Alternative strategies, such as lifestyle modifications, may be explored as safer options during pregnancy.
Statins and Menopause: A Consideration for Hormone Changes
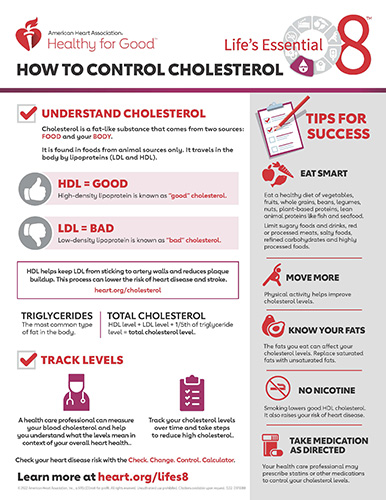
Menopause is a natural phase in a woman’s life that brings about hormonal changes, including a decrease in estrogen levels. These hormonal shifts can have an impact on cholesterol metabolism. In some women, menopause may lead to an increase in LDL cholesterol levels, which is a risk factor for heart disease.
Statins can be a valuable tool for managing elevated cholesterol levels in menopausal women. However, it is essential for healthcare providers to take into account the individual’s overall health, risk factors, and potential side effects when considering statin therapy. Additionally, healthcare providers should discuss with their patients the potential interactions between statins and hormone replacement therapy (HRT), if HRT is being used to manage menopausal symptoms.
Patient-Centered Decision-Making
The key takeaway from considering statin use in women’s health is that decisions should be patient-centered and based on a thorough evaluation of each woman’s unique health profile. Factors such as age, cholesterol levels, family history, and individual health goals all play a role in determining the appropriateness of statin therapy.
Open and informed discussions between healthcare providers and their female patients are crucial. These conversations should include a thorough assessment of potential risks and benefits, alternatives to statin therapy, and lifestyle modifications that can complement any prescribed treatment.
In conclusion, statins have undeniably made significant contributions to cardiovascular health in both men and women. However, when it comes to women’s health, considerations related to pregnancy and menopause require careful evaluation and personalized decision-making. Healthcare providers should collaborate with their patients to ensure that statin therapy is tailored to individual needs while prioritizing both the woman’s health and, if applicable, the health of the developing fetus during pregnancy. By adopting a patient-centered approach, we can strike a balance between managing cholesterol effectively and maintaining the well-being of women at every stage of life.
Additionally, you can find further information on this topic by visiting this page: Menopause Transition and Cardiovascular Disease Risk …
Statins are a class of medications primarily prescribed to lower LDL (low-density lipoprotein) cholesterol, often referred to as “bad” cholesterol. They work by inhibiting an enzyme in the liver involved in cholesterol production, thereby reducing the risk of atherosclerosis and related cardiovascular events.
Statins represent a cornerstone in the realm of cardiovascular health, revered for their ability to combat one of the leading risk factors for heart disease: elevated LDL (low-density lipoprotein) cholesterol, commonly known as “bad” cholesterol. The mechanism behind statins’ efficacy lies in their remarkable capacity to target cholesterol at its source, the liver, ultimately contributing to a reduced risk of atherosclerosis and the associated cardiovascular complications.
At their core, statins are designed to inhibit an enzyme in the liver called HMG-CoA reductase. This enzyme plays a central role in the production of cholesterol within the body. When statins intervene and hinder the action of HMG-CoA reductase, they effectively reduce the liver’s ability to synthesize cholesterol. This, in turn, leads to a decrease in the overall levels of LDL cholesterol circulating in the bloodstream.
The significance of this reduction cannot be overstated. Elevated LDL cholesterol is a primary contributor to the development of atherosclerosis, a progressive condition characterized by the buildup of cholesterol-rich plaques within the walls of arteries. These plaques can narrow and harden the arteries, impeding the flow of blood and increasing the risk of blockages. When blockages occur in critical arteries supplying the heart or brain, they can trigger life-threatening events such as heart attacks and strokes.
By lowering LDL cholesterol levels, statins effectively slow down the progression of atherosclerosis, reducing the likelihood of plaque formation and arterial blockages. This, in turn, translates into a decreased risk of cardiovascular events and the associated morbidity and mortality.
Furthermore, statins exhibit additional benefits beyond cholesterol management. They possess anti-inflammatory properties that can help stabilize existing plaques, making them less likely to rupture and cause sudden blockages. Statins also have a positive influence on endothelial function, which is vital for maintaining the health of the inner lining of blood vessels.
In essence, statins are more than just cholesterol-lowering medications; they are formidable allies in the fight against cardiovascular disease. Their ability to target cholesterol at its origin in the liver and exert a multi-faceted protective effect on the cardiovascular system underscores their significance in modern medicine. These medications, when prescribed judiciously and monitored appropriately, offer a potent means of reducing the risk of heart disease, improving overall heart health, and ultimately contributing to longer, healthier lives.
Looking for more insights? You’ll find them right here in our extended coverage: Statin Toxicity | Circulation Research
Pregnancy is a unique period in a woman’s life when considerations about medication safety take center stage. Statin use during pregnancy is a topic of concern due to potential risks to both the mother and the developing fetus:
Pregnancy marks a remarkable and transformative journey in a woman’s life, a time when the utmost care and attention are directed toward ensuring the well-being of both the mother and the developing fetus. In this delicate period, considerations about medication safety become paramount, and discussions about the risks and benefits of specific treatments are crucial. One such topic of concern in the realm of pregnancy is the use of statins, a class of medications commonly prescribed to manage cholesterol levels.
Statin use during pregnancy is a matter of significant medical scrutiny and caution, primarily because of the potential risks it poses to both the mother and the developing fetus. Statins are highly effective in lowering cholesterol levels, but their mechanisms of action can have unintended consequences when used during pregnancy.
For the mother, one of the primary concerns is the impact of statins on the developing fetus. These medications have the potential to cross the placental barrier, which means they can reach the developing baby’s bloodstream. While the precise effects of statins on fetal development are not fully understood, some studies suggest that they may be associated with birth defects and developmental abnormalities. This raises a red flag for healthcare providers who must weigh the potential benefits of statin therapy against the risks to the unborn child.
Additionally, statins could potentially affect the mother’s body in ways that are not conducive to a healthy pregnancy. Cholesterol plays a crucial role in the production of hormones, including those needed for a successful pregnancy. Lowering cholesterol levels with statins during pregnancy may disrupt these hormonal processes, potentially complicating the pregnancy and increasing the risk of complications.
Given these concerns, the use of statins during pregnancy is generally discouraged. Healthcare providers will explore alternative approaches to managing cholesterol levels in pregnant women, often focusing on dietary and lifestyle modifications to minimize potential risks.
In cases where a woman becomes pregnant while already taking statins, it is essential to communicate openly with healthcare providers. Together, they can carefully assess the risks and benefits of continuing or discontinuing statin therapy, making informed decisions that prioritize both maternal and fetal health.
In conclusion, pregnancy is a unique and precious period in a woman’s life that demands meticulous attention to medication safety. The use of statins during pregnancy remains a complex and challenging issue, with potential risks to both the mother and the developing fetus. It underscores the importance of thoughtful and informed discussions between healthcare providers and expectant mothers to make the best choices for a healthy pregnancy.
You can also read more about this here: 2019 ACC/AHA Guideline on the Primary Prevention of …

Given the potential risks, healthcare providers typically advise women to discontinue statin therapy when planning pregnancy or as soon as pregnancy is confirmed. Women with high cholesterol levels who are considering pregnancy should work closely with their healthcare providers to develop an alternative cholesterol management plan that prioritizes both maternal and fetal health.
The delicate balance between managing maternal health and safeguarding fetal well-being during pregnancy is a paramount concern for both women and their healthcare providers. While statins have proven efficacy in controlling cholesterol levels, their potential risks during pregnancy necessitate careful consideration and an alternative approach to cholesterol management.
Risk Mitigation in Pregnancy: Statins have the potential to cross the placenta, exposing the developing fetus to the medication. This exposure could potentially lead to adverse effects on fetal development, particularly in the early stages when organ formation is occurring. Therefore, healthcare providers typically recommend discontinuing statin therapy when pregnancy is planned or confirmed to mitigate these potential risks.
Collaborative Decision-Making: Women with high cholesterol levels who are contemplating pregnancy should engage in open and collaborative discussions with their healthcare providers. These discussions should encompass the risks associated with elevated cholesterol levels during pregnancy and the potential risks of statin use.
Alternative Management Plans: Developing an alternative cholesterol management plan tailored to the specific needs of the pregnant woman is crucial. Lifestyle modifications, such as dietary changes and exercise, can play a pivotal role in maintaining healthy cholesterol levels. Healthcare providers may also consider non-statin medications that have a more established safety profile during pregnancy if medication is deemed necessary.
Close Monitoring: Close monitoring of cholesterol levels during pregnancy is essential. Healthcare providers can perform regular blood tests to assess the maternal cholesterol profile and make necessary adjustments to the management plan as the pregnancy progresses.
Maternal and Fetal Health Prioritization: The overarching goal is to strike a balance that prioritizes both maternal and fetal health. Maintaining cholesterol levels within a safe range is important for maternal well-being, as excessively high cholesterol levels during pregnancy can pose risks such as gestational diabetes and preeclampsia. However, any intervention or medication used should prioritize fetal safety above all else.
Postpartum Considerations: After childbirth, healthcare providers can reevaluate the cholesterol management strategy and determine whether statin therapy should be resumed. This decision will depend on the woman’s cholesterol levels, overall health, and plans for future pregnancies.
In conclusion, the management of cholesterol levels during pregnancy involves a thoughtful and individualized approach. Given the potential risks, discontinuing statin therapy during pregnancy is a common practice, but it should be done in consultation with a healthcare provider. Developing an alternative cholesterol management plan, closely monitoring cholesterol levels, and prioritizing both maternal and fetal health are essential steps in ensuring a healthy pregnancy for women with high cholesterol levels.
To expand your knowledge on this subject, make sure to read on at this location: 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC …

Menopause marks a significant transition in a woman’s life, characterized by the cessation of menstruation and a decrease in estrogen levels. Estrogen plays a role in maintaining healthy cholesterol levels, and its decline during menopause can lead to changes in lipid profiles:
Menopause is a profound and inevitable milestone in a woman’s life, signifying the end of the reproductive years and often accompanied by a range of physical and hormonal changes. One of the key transformations during this period is the cessation of menstruation and a notable decrease in estrogen levels, a hormone that has far-reaching effects on various aspects of health, including cholesterol management.
Estrogen, often thought of as the quintessential female hormone, plays a multifaceted role in maintaining overall health. Among its many functions, estrogen has a hand in regulating cholesterol levels in the body. It tends to raise levels of high-density lipoprotein (HDL) cholesterol, often referred to as the “good” cholesterol, while also helping to keep low-density lipoprotein (LDL) cholesterol, the “bad” cholesterol, in check. This delicate balance contributes to a healthier lipid profile and a lower risk of atherosclerosis, a condition characterized by the buildup of fatty deposits in the arteries.
However, with the onset of menopause, estrogen production takes a significant dip. This hormonal shift can have a notable impact on a woman’s cholesterol levels and overall cardiovascular health. The decline in estrogen levels is often associated with changes in lipid profiles. LDL cholesterol levels may increase, while HDL cholesterol levels may decrease. This shift in the lipid profile can, in turn, elevate the risk of heart disease and other cardiovascular conditions.
Moreover, menopausal women may also experience changes in the distribution of body fat. Fat tends to accumulate more in the abdominal area, which is associated with a higher risk of heart disease. These changes in body composition, coupled with alterations in lipid profiles, underscore the need for proactive cardiovascular care during menopause.
In light of these hormonal fluctuations, it becomes imperative for women transitioning through menopause to be vigilant about their heart health. Regular check-ups, cholesterol screenings, and discussions with healthcare providers are essential to monitor and manage cholesterol levels effectively. Lifestyle adjustments, such as a heart-healthy diet and regular physical activity, can be particularly beneficial in mitigating the impact of menopause-related changes on cardiovascular health.
In conclusion, menopause heralds a significant period of change in a woman’s life, not only marked by the cessation of menstruation but also by a shift in hormone levels, notably estrogen. Understanding the interplay between estrogen and cholesterol is crucial, as the decline in estrogen during menopause can lead to alterations in lipid profiles that may increase the risk of heart disease. By staying informed and proactive about heart health during this transitional phase, women can navigate menopause with confidence, safeguarding their cardiovascular well-being for years to come.
Explore this link for a more extensive examination of the topic: Cholesterol Management in Women: What Does the 2018 Guideline …

The use of statins in women’s health requires careful consideration, particularly during pregnancy and menopause. Balancing the benefits of cholesterol management with potential risks is essential for both maternal and fetal well-being during pregnancy, and for cardiovascular health during menopause.
Women should engage in open and informed discussions with their healthcare providers about statin therapy, especially if they are planning a pregnancy or undergoing menopause. These conversations can help women make well-informed decisions that align with their unique health profiles, ultimately promoting better cardiovascular health and overall well-being.
Don’t stop here; you can continue your exploration by following this link for more details: Women’s involvement in clinical trials: historical perspective and …
More links
Additionally, you can find further information on this topic by visiting this page: Dyslipidemia in women: etiology and management – PMC
