Introduction
Statins, a class of medications widely prescribed for cholesterol management, have long been the subject of scientific investigation regarding their potential impact on cognitive health. While the primary purpose of statins is to lower cholesterol and reduce cardiovascular risk, some studies have suggested a link between statin use and memory-related effects. In this article, we will explore the evidence surrounding statins and their potential influence on cognitive function and memory.
Statins, a class of medications that have earned their place in the spotlight for their effectiveness in managing cholesterol levels and reducing cardiovascular risk, have also piqued scientific curiosity when it comes to their potential impact on cognitive health. While the primary role of statins is to target and lower cholesterol, researchers have undertaken investigations into whether there might be a connection between statin use and memory-related effects. In this article, we embark on a journey into the realm of scientific inquiry, aiming to shed light on the existing evidence surrounding statins and their potential influence on cognitive function and memory.
Exploring the Cognitive Frontier: The study of statins and cognition is akin to exploring a relatively uncharted territory in the vast landscape of medical research. While the primary focus has always been on the cardiovascular benefits of these medications, the potential ripple effects on cognitive function have raised intriguing questions.
Complex and Evolving Landscape: The relationship between statin use and cognitive health is a complex and evolving area of study. Some research has suggested that statins might have a protective effect on cognitive function, potentially reducing the risk of cognitive decline and neurodegenerative conditions like Alzheimer’s disease. Conversely, other studies have hinted at potential memory-related side effects associated with statin use.
The Evidence Thus Far: Research findings in this field are nuanced, and the evidence remains mixed. Some studies have reported no significant adverse cognitive effects associated with statin use, while others have noted potential concerns, such as mild memory impairment or cognitive changes.
Individual Variability: It’s essential to recognize that individual responses to statins can vary widely. Factors such as age, genetics, and overall health may influence how a person responds to these medications concerning cognitive function. For some, statins may have no discernible impact on memory or cognitive abilities, while others might experience changes, positive or negative.
Balancing Act: The critical challenge lies in striking the right balance between the well-established cardiovascular benefits of statins and any potential cognitive effects. It’s important to emphasize that cardiovascular health should remain the primary focus of statin therapy, especially for individuals at high risk of heart disease.
The Role of Informed Decision-Making: In this context, informed decision-making is paramount. Patients and healthcare providers must engage in open and thoughtful discussions regarding the use of statins, weighing the potential benefits against any perceived cognitive risks. This collaborative approach ensures that the course of treatment aligns with individual health goals and concerns.
Future Directions: As the field of research on statins and cognition continues to evolve, future studies may provide more definitive insights into this complex relationship. These findings could pave the way for personalized treatment approaches that consider both cardiovascular health and cognitive well-being.
In conclusion, while the primary purpose of statins is to lower cholesterol and reduce cardiovascular risk, the question of their potential impact on cognitive health adds a layer of intrigue to the broader conversation. As we navigate this scientific terrain, it’s essential to remain open to new discoveries, prioritize cardiovascular health, and engage in informed discussions with healthcare providers to make decisions that align with individual health goals and concerns.
To delve further into this matter, we encourage you to check out the additional resources provided here: The role of statins in both cognitive impairment and protection …
Before delving into the cognitive effects of statins, it’s essential to understand their primary function. Statins work by inhibiting an enzyme in the liver responsible for cholesterol production, ultimately leading to lower LDL (low-density lipoprotein) cholesterol levels in the bloodstream. This reduction in LDL cholesterol is crucial for reducing the risk of atherosclerosis and cardiovascular events like heart attacks and strokes.
Before we embark on exploring the potential cognitive effects of statins, it’s crucial to grasp their fundamental mechanism of action and why they have become such a cornerstone in cardiovascular care. Statins, as a class of medications, exert their primary effect by inhibiting an enzyme in the liver known as HMG-CoA reductase. This enzyme plays a pivotal role in the production of cholesterol within the body, particularly LDL (low-density lipoprotein) cholesterol—the infamous “bad” cholesterol that is notorious for its role in atherosclerosis and the development of cardiovascular diseases.
When statins step onto the scene, they act as regulators of this cholesterol production line, slowing it down significantly. This, in turn, leads to a marked reduction in the levels of LDL cholesterol circulating in the bloodstream. It’s this precise mechanism that forms the bedrock of their effectiveness in cardiovascular health.
By diligently lowering LDL cholesterol, statins offer a formidable shield against the progression of atherosclerosis—a condition characterized by the buildup of fatty plaques in the arteries. These plaques can narrow blood vessels, reducing blood flow and increasing the risk of blood clots, heart attacks, and strokes. Statins, with their cholesterol-lowering prowess, thus stand as formidable guardians of heart health.
This understanding of statins’ primary function underscores their significance in preventing and managing cardiovascular events. As we delve further into the potential cognitive effects of statins, it’s this foundational knowledge that will help us navigate the complexities of their role in brain health, ensuring a comprehensive view of their impact on overall well-being.
Looking for more insights? You’ll find them right here in our extended coverage: The role of statins in both cognitive impairment and protection …
The notion that statin use might affect cognitive health has sparked considerable interest and debate among researchers, healthcare providers, and the public. Here are some key points to consider:
The intersection of statin use and cognitive health has become a focal point of intrigue, debate, and discussion, captivating the attention of researchers, healthcare providers, and the general public alike. Amidst this complex landscape, it’s essential to navigate the topic with a balanced perspective, taking into account various facets and nuances. Here are some key points to consider:
Diverse Findings in Research: The relationship between statins and cognitive health is multifaceted. While some studies have raised concerns about potential cognitive side effects, others have found no significant adverse effects on memory or cognitive function. It’s important to recognize that research outcomes can vary, and interpreting these findings requires a nuanced approach.
Individual Variability: Individuals may respond differently to statin therapy. Some people may report cognitive symptoms, such as memory problems or confusion, while taking statins, while others may not experience any noticeable changes. Understanding this variability is essential when evaluating the impact of statins on cognitive health.
Benefits vs. Risks: Statins are widely prescribed for their well-established benefits in lowering cholesterol and reducing the risk of heart disease. For many individuals, the cardiovascular advantages of statins far outweigh the potential risks related to cognitive function. Balancing these factors is a crucial consideration in clinical decision-making.
Possible Mechanisms: Researchers are actively exploring the mechanisms through which statins might influence cognitive health. Some theories suggest that statins could affect brain function through their impact on cholesterol metabolism, inflammation, or blood flow. However, these mechanisms are not yet fully understood.
Shared Decision-Making: The decision to start, continue, or discontinue statin therapy should involve open and informed discussions between patients and healthcare providers. Considering an individual’s overall health, cardiovascular risk factors, and any potential cognitive concerns is essential in making personalized treatment decisions.
Monitoring and Awareness: Regular monitoring of cognitive function can be part of responsible statin therapy. Healthcare providers may assess cognitive health during routine check-ups, and patients are encouraged to report any cognitive symptoms they experience while taking statins.
Lifestyle Factors: Lifestyle choices, such as diet, exercise, and managing other health conditions, also play a significant role in cognitive health. Addressing these factors alongside statin therapy can contribute to overall well-being.
In conclusion, the relationship between statin use and cognitive health is a complex and evolving field of study. It’s important to approach the topic with a balanced perspective, acknowledging the potential variability in individual responses and the well-established cardiovascular benefits of statins. In shared decision-making with healthcare providers, patients can make informed choices that prioritize both heart health and cognitive well-being. As ongoing research sheds further light on this issue, our understanding will continue to evolve, guiding more tailored approaches to statin therapy.
Should you desire more in-depth information, it’s available for your perusal on this page: PCSK9 Inhibitors and Neurocognitive Adverse Events: Exploring the …
Research investigating the relationship between statin use and cognitive function has yielded mixed results. While some studies have suggested a potential link between statin use and cognitive decline or memory-related effects, others have found no significant association.
The complex relationship between statin use and cognitive function has been the subject of extensive research, and the findings have indeed been mixed, adding layers of nuance to our understanding of this critical topic. As we navigate this intricate landscape, several key insights have emerged:
Potential Concerns: Some studies have raised potential concerns regarding the impact of statin use on cognitive function. These concerns primarily center around reports of cognitive decline or memory-related effects among a subset of statin users. While these findings have garnered attention, it’s essential to recognize that these effects are generally modest and not experienced by the majority of patients.
No Significant Association: Contrary to the concerns raised by some studies, a substantial body of research has found no significant association between statin use and cognitive decline. These findings emphasize that for most individuals, statin therapy does not adversely affect cognitive function.
Individual Variability: The relationship between statins and cognitive function appears to be highly individualized. Factors such as age, genetics, existing cognitive health, and the specific type of statin used can influence how a person responds to this medication class.
Beneficial Effects: Intriguingly, some studies have suggested that statin use may have potential cognitive benefits, particularly in populations at higher risk of cognitive decline due to cardiovascular risk factors. The cardiovascular benefits of statins, including improved blood flow and reduced risk of stroke, may indirectly support cognitive health.
Shared Decision-Making: As with any medical treatment, the decision to prescribe statins should be made through shared decision-making between healthcare providers and patients. This approach enables open discussions about potential risks and benefits, allowing for individualized treatment plans that align with the patient’s overall health goals.
In essence, the relationship between statin use and cognitive function remains a topic of ongoing research and debate. While concerns have been raised, it’s crucial to consider the broader context: for most individuals, statins provide substantial cardiovascular benefits while having little to no adverse impact on cognitive function. This nuanced perspective encourages healthcare providers and patients to engage in informed conversations about statin therapy, ensuring that treatment decisions prioritize both heart health and cognitive well-being.
Should you desire more in-depth information, it’s available for your perusal on this page: Modifiable Midlife Risk Factors for Late-Life Cognitive Impairment …
The exact mechanisms by which statins might influence cognitive health are not fully understood. Some hypotheses suggest that statins could affect the production of cholesterol in the brain, which plays a role in synaptic function and memory.
The exact mechanisms by which statins might influence cognitive health continue to be an area of active research, and while several hypotheses exist, a comprehensive understanding has yet to emerge. One of the intriguing theories under consideration is that statins could impact cognitive function through their effects on cholesterol metabolism within the brain. Here are some key aspects to consider:
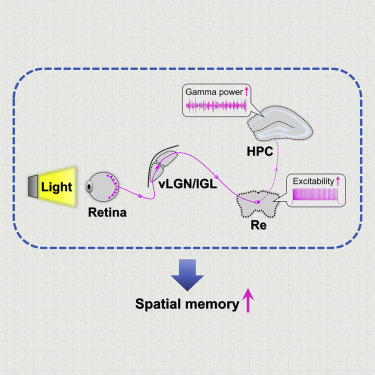
Cholesterol in the Brain: Cholesterol is not only present in our bloodstream but also in our brain, where it plays a crucial role in various processes, including synaptic function and the formation of cell membranes. In the brain, cholesterol is involved in the creation of myelin, a substance that insulates nerve fibers, and it’s also essential for the maintenance of neuronal connections.
Statins and Brain Cholesterol: Statins are primarily known for their ability to lower cholesterol levels in the bloodstream by inhibiting HMG-CoA reductase, an enzyme involved in cholesterol production. Some researchers posit that statins could have a similar effect on cholesterol production in the brain. If this were the case, it might influence the availability of cholesterol for essential brain functions.
Synaptic Function: Synapses are the connections between neurons, where information is transmitted through chemical signals. Cholesterol is involved in maintaining the integrity of these synapses and may influence synaptic plasticity, which is essential for learning and memory. Statins potentially altering brain cholesterol levels could thus affect synaptic function.
Memory and Cognition: Memory formation and cognitive processes rely on the efficient transmission of signals between neurons. Any disruption in synaptic function or connectivity due to changes in brain cholesterol could potentially impact memory and cognitive abilities.
Variability in Response: It’s important to note that the impact of statins on brain cholesterol levels and cognitive function can vary from person to person. Individual factors, including genetics, overall health, and lifestyle, may influence how statins affect the brain. This variability adds complexity to understanding the relationship.
Ongoing Research: Researchers are actively investigating these hypotheses and conducting clinical trials to gain a clearer understanding of the potential connections between statins, brain cholesterol, and cognitive health. Ongoing studies aim to elucidate who might be more susceptible to cognitive effects and under what circumstances.
In conclusion, while the exact mechanisms remain elusive, the theory that statins might influence cognitive health through their effects on brain cholesterol is a compelling area of research. It underscores the importance of continued exploration into the potential interactions between statin therapy and cognitive function, as well as the need for personalized healthcare approaches that consider individual factors when prescribing statins. Further research will likely contribute to a more comprehensive understanding of this complex relationship.
Don’t stop here; you can continue your exploration by following this link for more details: Dementia prevention, intervention, and care: 2020 report of the …
Responses to statin therapy vary among individuals. Some people may experience cognitive changes while taking statins, while others may not. Genetic factors, underlying health conditions, and lifestyle factors can contribute to this variability.
Responses to statin therapy indeed exhibit significant variability among individuals. This diversity in reactions to statins underscores the importance of personalized healthcare and understanding the multifaceted factors that influence these responses.
Genetic factors play a substantial role in determining how individuals metabolize and respond to statin medications. Genetic variations can affect the enzymes responsible for breaking down statins in the body, potentially leading to differences in drug levels and efficacy. Additionally, genetics can influence how the body processes cholesterol and manages lipid profiles, which further contributes to the variation in statin responses.
Underlying health conditions also contribute to this diversity. Individuals with comorbidities such as diabetes, kidney disease, or liver dysfunction may respond differently to statin therapy. These conditions can influence how the body handles medications, potentially impacting both the effectiveness and side effects of statins.
Lifestyle factors are another significant variable. Diet, exercise, and overall lifestyle choices can influence how statins interact with the body. For example, a heart-healthy diet and regular physical activity can complement statin therapy, enhancing its effectiveness and potentially mitigating side effects. Conversely, a sedentary lifestyle or a diet high in saturated fats can hinder the benefits of statins and increase the risk of side effects.
Age also plays a role in the variability of statin responses. Older individuals may experience different reactions to statins compared to younger ones due to age-related changes in metabolism and potential interactions with other medications commonly taken by older adults.
Understanding and addressing these factors is crucial in optimizing statin therapy for each individual. Healthcare providers should conduct a comprehensive assessment of patients, taking into account their genetic background, existing health conditions, lifestyle choices, and age to make informed decisions about statin treatment.
Moreover, open communication between healthcare providers and patients is essential. Patients should be encouraged to report any unusual symptoms or side effects they experience while on statins promptly. This feedback can help healthcare providers tailor treatment plans, potentially adjusting dosages or exploring alternative medications to achieve the desired cholesterol management goals while minimizing side effects.
In summary, recognizing the variability in responses to statin therapy and considering the interplay of genetic, health, and lifestyle factors is key to achieving the best outcomes for individuals. This personalized approach ensures that statin treatment is both effective and well-tolerated, ultimately promoting better cardiovascular health.
Should you desire more in-depth information, it’s available for your perusal on this page: Association of Video Gaming With Cognitive Performance Among …
It’s important to consider the broader context. Statins are prescribed primarily for their cardiovascular benefits, which are well-established. The potential cognitive effects, even if present, must be weighed against the known benefits of statin therapy in reducing heart disease and stroke risk.
Considering the broader context is essential when evaluating the use of statins in healthcare. These medications have been primarily prescribed for their well-established cardiovascular benefits, which are backed by extensive research and clinical evidence. Statins have consistently proven their effectiveness in lowering LDL (low-density lipoprotein) cholesterol levels, reducing the risk of atherosclerosis, heart disease, and stroke. However, it’s crucial to approach any potential side effects, including cognitive effects, within this context.
While some studies have suggested a possible link between statin use and cognitive changes, the overall evidence remains mixed and inconclusive. It’s essential to recognize that correlation does not necessarily imply causation, and the cognitive effects observed in some individuals may be due to various factors other than statin use. These potential cognitive effects, even if present, must be weighed against the substantial and well-documented benefits of statin therapy.
The benefits of statins in reducing heart disease and stroke risk cannot be overstated. They have played a pivotal role in preventing countless cardiovascular events and saving lives worldwide. Statins work by lowering LDL cholesterol levels, which are a key contributor to the development of atherosclerosis, the buildup of plaque in arteries. By reducing this risk factor, statins help maintain clear and healthy arteries, reducing the likelihood of heart attacks and strokes.
Furthermore, statins often benefit individuals with a history of cardiovascular disease or those at a high risk of developing it. They can stabilize existing plaque, prevent its progression, and even promote plaque regression in some cases. Additionally, statins have anti-inflammatory properties that contribute to their cardiovascular protective effects.
Given the overwhelming evidence supporting the cardiovascular benefits of statins, healthcare providers carefully consider the risk-to-benefit ratio when prescribing these medications. They take into account an individual’s cholesterol levels, overall cardiovascular risk profile, and any potential side effects, including cognitive concerns. In most cases, the potential cognitive effects are outweighed by the significant reduction in the risk of life-threatening cardiovascular events.
It’s essential for patients and healthcare providers to engage in open and informed discussions about statin therapy. Any concerns about potential side effects, including cognitive effects, should be addressed, and decisions regarding treatment should be made collaboratively, considering the individual’s unique health circumstances and goals.
In conclusion, while the potential cognitive effects of statins may be a topic of discussion and ongoing research, their cardiovascular benefits remain well-established and undeniable. The decision to use statin therapy should be based on a comprehensive assessment of an individual’s cardiovascular risk and the potential benefits in reducing heart disease and stroke risk. The ultimate goal is to maximize overall health and well-being while minimizing risks.
Should you desire more in-depth information, it’s available for your perusal on this page: Ginkgo – Mayo Clinic

Healthcare providers should engage in shared decision-making with patients when prescribing statins. This involves discussing potential risks and benefits and considering individual patient characteristics and preferences.
Shared decision-making between healthcare providers and patients is at the core of patient-centered care, especially when it comes to prescribing medications like statins. It’s not just a consultation; it’s a collaborative process that acknowledges the importance of the patient’s voice in their own healthcare journey.
To achieve this, healthcare providers should foster open and transparent communication with their patients. They should take the time to discuss the potential risks and benefits associated with statin use in a comprehensible and patient-friendly manner. This means breaking down complex medical jargon into simple terms, ensuring that patients fully grasp the implications of their treatment choices.
Moreover, shared decision-making goes beyond providing information. It involves actively listening to patients’ concerns, preferences, and values. Each patient is unique, and what matters most to one person might differ from another. Some may prioritize reducing their risk of heart disease, while others may be more concerned about potential side effects. By acknowledging these individual perspectives, healthcare providers can tailor their recommendations to align with the patient’s goals and values.
Patient characteristics also play a pivotal role in this process. Age, gender, medical history, and lifestyle factors can all influence the decision to prescribe statins. Healthcare providers should take these factors into account when discussing treatment options, as they can impact both the potential benefits and risks of statin therapy.
Ultimately, the goal of shared decision-making is to arrive at a treatment plan that the patient feels comfortable with and committed to. When patients are actively involved in the decision-making process, they tend to be more engaged in their own care, leading to better adherence to treatment plans and improved health outcomes.
In conclusion, shared decision-making empowers patients and recognizes their right to be active participants in their healthcare decisions. It transforms the patient-provider relationship into a partnership, ensuring that the chosen treatment aligns with the patient’s values, preferences, and individual characteristics. This collaborative approach not only enhances the quality of care but also respects the autonomy and dignity of each patient, making healthcare a truly patient-centered experience.
To expand your knowledge on this subject, make sure to read on at this location: Interventions for increasing the use of shared decision making by …

The relationship between statin use and cognitive health remains an area of ongoing research and discussion. While some studies have suggested associations between statin use and memory-related effects, the evidence is not conclusive, and the observed effects, if present, tend to be subtle.
It’s essential for patients and healthcare providers to engage in open and informed discussions when considering statin therapy. The potential cognitive effects, even if real, should be weighed against the well-established cardiovascular benefits of statins. Additionally, other factors, such as genetics and lifestyle, may contribute to individual variations in cognitive response to statins.
Ultimately, the decision to use statins should be made on a case-by-case basis, with careful consideration of the patient’s cardiovascular risk profile, preferences, and potential concerns about cognitive health. Further research will continue to shed light on the complex relationship between statins and cognitive function, providing a more comprehensive understanding of this intriguing topic.
Don’t stop here; you can continue your exploration by following this link for more details: Risk reduction of cognitive decline and dementia: WHO guidelines
More links
To delve further into this matter, we encourage you to check out the additional resources provided here: Dementia prevention, intervention, and care: 2020 report of the …
