Introduction
Statin medications have become a cornerstone in the management of high cholesterol levels, significantly reducing the risk of heart disease. While these drugs are highly effective, they can interact with other medications, potentially leading to adverse effects or reduced efficacy. In this article, we will explore the essential information you need to know about statin drug interactions to ensure the safe and effective use of these cholesterol-lowering drugs.
Statin medications have become a cornerstone in the management of high cholesterol levels, significantly reducing the risk of heart disease. While these drugs are highly effective, they can interact with other medications, potentially leading to adverse effects or reduced efficacy. In this article, we will explore the essential information you need to know about statin drug interactions to ensure the safe and effective use of these cholesterol-lowering drugs.
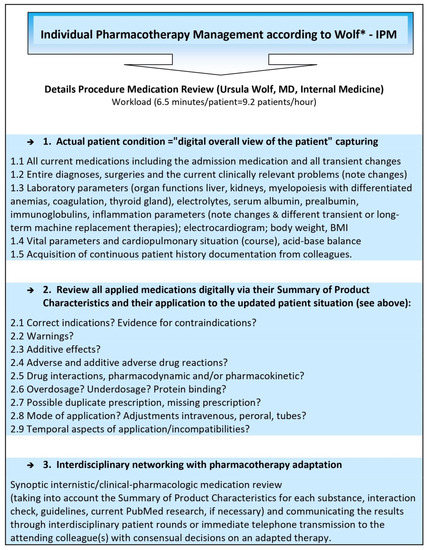
Common Interactions: Statins can interact with a range of medications, including those prescribed for blood pressure, diabetes, and blood thinning. It’s crucial to understand how statins may affect these medications and vice versa to prevent any unintended consequences.
Blood Pressure Medications: Some blood pressure medications may interact with statins, affecting blood pressure control. Your healthcare provider can help you find the right combination or adjust dosages to maintain both your cholesterol and blood pressure at optimal levels.
Diabetes Medications: For individuals managing diabetes, it’s essential to monitor blood sugar levels when taking statins. Statins may lead to a slight increase in blood sugar, so close collaboration with your healthcare team is vital to adjust diabetes medications as needed.
Blood Thinners: If you’re on blood thinning medications, be aware that statins can increase the risk of bleeding. Your doctor will carefully assess the balance between managing cholesterol and minimizing bleeding risk, often adjusting medication doses accordingly.
Liver Function: Statins are processed in the liver, so any medication that affects liver function can potentially interact with them. Regular liver function tests are typically recommended when taking statins to ensure they are well-tolerated.
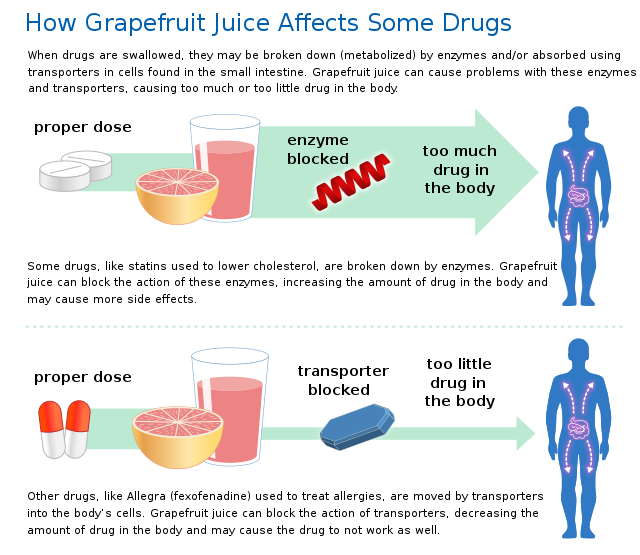
Over-the-Counter Supplements: Even supplements like grapefruit juice and certain herbal products can interact with statins. Grapefruit juice, for example, can increase statin levels in your bloodstream, potentially leading to adverse effects. Always discuss the use of supplements with your healthcare provider.
Personalized Assessment: Keep in mind that the impact of statin interactions can vary from person to person based on factors like genetics and overall health. Your healthcare provider will conduct a personalized assessment to determine the most suitable statin and dosage for you.
Open Communication: Effective communication with your healthcare provider is vital. Make sure to inform them of all medications, supplements, and even vitamins you are taking to create a comprehensive and safe treatment plan.
Regular Monitoring: Continuous monitoring of your cholesterol levels, along with potential side effects or interactions, is essential. Regular check-ups and blood tests help your healthcare team make necessary adjustments to your statin therapy.
Lifestyle Considerations: Alongside medications, a heart-healthy lifestyle, including a balanced diet, regular exercise, and stress management, plays a crucial role in managing cholesterol levels. Combining these lifestyle changes with statin therapy can further enhance their effectiveness.
In conclusion, while statin medications are powerful tools for managing high cholesterol, their interactions with other drugs require careful consideration. Your healthcare provider is your best resource for navigating these interactions, ensuring that you receive the maximum benefit from statins while minimizing potential risks. Always consult with them before starting or changing any medication regimen involving statins.
To expand your knowledge on this subject, make sure to read on at this location: Niacin – Health Professional Fact Sheet
Statin medications, such as atorvastatin (Lipitor), simvastatin (Zocor), and rosuvastatin (Crestor), work by inhibiting the enzyme HMG-CoA reductase, which is involved in cholesterol production in the liver. By lowering LDL (low-density lipoprotein) cholesterol levels, they help reduce the risk of heart attacks and strokes.
Statin medications, such as atorvastatin (Lipitor), simvastatin (Zocor), and rosuvastatin (Crestor), are widely prescribed for their ability to effectively manage cholesterol levels and, in turn, lower the risk of heart disease and stroke. These medications work by targeting a key player in the cholesterol production process within the body: the enzyme HMG-CoA reductase.
HMG-CoA reductase is responsible for the synthesis of cholesterol in the liver. When you consume dietary cholesterol and saturated fats, your liver produces even more cholesterol, leading to elevated levels of LDL (low-density lipoprotein) cholesterol in your bloodstream. High LDL cholesterol is a significant risk factor for the development of atherosclerosis, a condition characterized by the buildup of plaque in your arteries, potentially leading to heart attacks and strokes.
Statin medications act as a powerful tool to combat this process. By inhibiting HMG-CoA reductase, they essentially block the production of cholesterol in the liver. This results in a significant reduction in LDL cholesterol levels circulating in the blood. Lowering LDL cholesterol is crucial because it directly contributes to the prevention of atherosclerosis and its associated cardiovascular complications.
Beyond their LDL-lowering effects, statins have been shown to provide additional benefits for heart health. They can stabilize existing plaque deposits in the arteries, making them less likely to rupture and cause a heart attack or stroke. Statins also have anti-inflammatory properties that can help reduce the overall inflammation in the cardiovascular system, further reducing the risk of these serious events.
It’s important to note that while statins are highly effective, they are typically prescribed based on an individual’s specific cholesterol profile and overall cardiovascular risk. Your healthcare provider will assess your unique situation and determine the most appropriate statin type and dosage for you. Additionally, statins are often part of a comprehensive approach to heart health, which may include lifestyle modifications like diet and exercise.
Regular monitoring and communication with your healthcare provider are key when taking statin medications to ensure that your cholesterol levels are well-managed and that any potential side effects are addressed promptly. By understanding how statins work and their role in cholesterol management, you can make informed decisions about your cardiovascular health in consultation with your healthcare team.
Additionally, you can find further information on this topic by visiting this page: Understanding the critical disposition pathways of statins to assess …
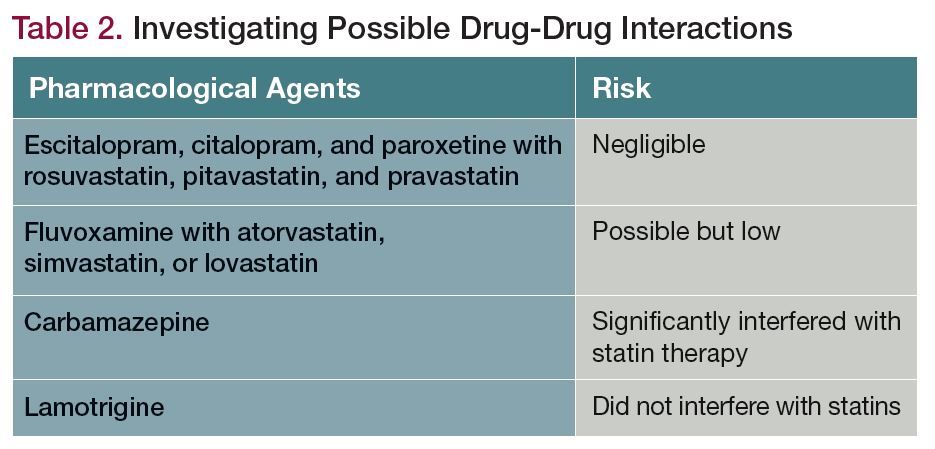
One of the most well-known interactions is between grapefruit juice and certain statins, particularly simvastatin and atorvastatin. Grapefruit juice can inhibit the metabolism of these drugs, leading to higher blood levels and an increased risk of side effects.
One of the most well-known interactions is between grapefruit juice and certain statins, particularly simvastatin and atorvastatin. Grapefruit juice can inhibit the metabolism of these drugs, leading to higher blood levels and an increased risk of side effects. This interaction serves as a striking example of how everyday foods and beverages can influence the way our bodies process medications.
The culprit in grapefruit juice is a group of compounds called furanocoumarins, which interfere with the activity of enzymes in the liver responsible for breaking down drugs. When these enzymes are inhibited, the body retains higher levels of the statins, which can result in an amplified response to the medication. This, in turn, increases the likelihood of experiencing side effects, such as muscle pain and weakness, known as myopathy or rhabdomyolysis, a severe and potentially life-threatening condition.
The intensity of the interaction can vary depending on several factors, including the individual’s metabolism, the specific statin taken, and the amount of grapefruit juice consumed. However, to err on the side of caution, many healthcare providers advise patients taking statins to avoid grapefruit and its juice altogether, especially if they are on medications like simvastatin or atorvastatin.
It’s important to recognize that the grapefruit-drug interaction is not limited to statins alone. Various other medications, including those used for blood pressure control, psychiatric conditions, and certain anti-inflammatories, can also be affected by grapefruit juice in a similar manner. This underscores the significance of discussing your dietary habits, including grapefruit consumption, with your healthcare provider when prescribed new medications.
In summary, the grapefruit juice interaction with statins serves as a powerful reminder of the intricate relationship between diet and medication. To ensure the safe and effective use of medications, always communicate openly with your healthcare provider about your dietary choices and potential interactions, and follow their guidance to optimize your treatment plan.
To expand your knowledge on this subject, make sure to read on at this location: Does grapefruit affect my medicine? – NHS
Some antibiotics, like erythromycin and clarithromycin, can interact with statins, potentially increasing the risk of muscle-related side effects.
It’s essential to be vigilant about potential interactions between medications, especially when it comes to your statin therapy. Certain antibiotics, such as erythromycin and clarithromycin, can inadvertently complicate your cardiovascular health journey.
These antibiotics, while effective in treating bacterial infections, have been found to interact with statins, posing an increased risk of muscle-related side effects. Statins are well-known for their cholesterol-lowering abilities, but they can also affect your muscle tissues. When combined with erythromycin or clarithromycin, the risk of muscle-related issues, known as myopathy or rhabdomyolysis, can rise.
Myopathy can manifest as muscle pain, tenderness, and weakness, which can be uncomfortable and limit your daily activities. In severe cases, it may escalate to rhabdomyolysis, where damaged muscle fibers release proteins into the bloodstream, potentially leading to kidney damage and other complications.
The interaction between these antibiotics and statins occurs because both are metabolized in the liver by the same enzyme pathway. When you take them together, it can disrupt this pathway, leading to an accumulation of statins in your bloodstream. This elevated statin concentration can heighten the risk of muscle problems.
If your healthcare provider prescribes erythromycin or clarithromycin while you are on statin therapy, it’s crucial to inform them of your statin use. They can assess the potential risks and benefits, and if necessary, may recommend an alternative antibiotic or adjust your statin dose to minimize the risk of adverse effects.
Understanding these medication interactions and communicating openly with your healthcare team is pivotal in ensuring your statin therapy effectively manages your cholesterol levels while minimizing potential complications. It’s another reminder of the importance of actively participating in your healthcare decisions and maintaining an open dialogue with your medical professionals.
For a comprehensive look at this subject, we invite you to read more on this dedicated page: Paxlovid Drug-Drug Interactions | COVID-19 Treatment Guidelines
Certain antifungal drugs, such as itraconazole and ketoconazole, can interact with statins, leading to elevated statin levels in the blood.
The interplay between medications can sometimes be a complex puzzle, and it’s essential to understand how certain drugs can affect one another. In the realm of medication interactions, it’s worth noting that antifungal drugs, particularly itraconazole and ketoconazole, have the potential to significantly impact the effectiveness and safety of statins, a class of medications often prescribed to manage cholesterol levels.
These antifungal drugs, while valuable in treating fungal infections, can interact with statins in a way that leads to elevated statin levels circulating in the bloodstream. This interaction occurs because both itraconazole and ketoconazole inhibit the enzymes responsible for breaking down statins in the liver. As a result, statins can accumulate in the body, increasing their potency and the risk of potential side effects.
The consequences of elevated statin levels due to these interactions can be twofold. On one hand, it might enhance the cholesterol-lowering effect of statins, which could be advantageous for individuals with high cholesterol levels. However, the flip side is that it also heightens the risk of statin-related side effects, particularly muscle-related issues such as myalgia (muscle pain) and, in severe cases, rhabdomyolysis (muscle breakdown).
Therefore, if you find yourself in a situation where you require antifungal treatment and are already taking statins, it’s vital to communicate openly with your healthcare provider. They can make necessary adjustments to your medication regimen, possibly opting for alternative antifungal options or modifying your statin dosage to mitigate potential interactions and minimize the risk of side effects.
Additionally, it underscores the importance of healthcare professionals having a comprehensive understanding of a patient’s medication history and ongoing treatments. This knowledge enables them to make informed decisions and tailor medical interventions to the individual’s specific needs, ensuring both the efficacy and safety of the prescribed therapies.
In conclusion, while antifungal medications like itraconazole and ketoconazole are valuable tools in treating fungal infections, their potential interactions with statins serve as a reminder of the intricate web of pharmaceutical interactions. Open communication with healthcare providers, thorough medication reviews, and personalized adjustments are essential to manage and minimize the risks associated with these interactions, ultimately ensuring the best possible outcomes for patients.
Additionally, you can find further information on this topic by visiting this page: Drug Interaction Checker – Find Interactions Between Medications

Drugs like amiodarone (used for heart arrhythmias) and verapamil (used for high blood pressure and heart conditions) may interact with statins, increasing the risk of side effects.
Drugs like amiodarone and verapamil, though vital for managing heart arrhythmias, high blood pressure, and various heart conditions, can sometimes introduce complexities when taken alongside statins. This interaction highlights the importance of close monitoring and medical guidance when managing multiple medications.
Amiodarone, a potent antiarrhythmic medication, can interfere with the metabolism of statins in the liver. Specifically, it may inhibit the activity of enzymes responsible for breaking down statins. As a result, statin levels in the bloodstream can rise significantly, increasing the risk of adverse effects, particularly muscle-related side effects like myopathy and rhabdomyolysis. It’s essential for healthcare providers to carefully select the appropriate statin and dosage when prescribed alongside amiodarone, ensuring a balance between therapeutic benefits and potential risks.
Verapamil, often used to treat high blood pressure and certain heart conditions, can also impact the metabolism of statins. It may inhibit the same liver enzymes as amiodarone, potentially leading to elevated statin concentrations in the blood. This elevation raises concerns about an increased risk of side effects, particularly for statins that have a narrow therapeutic window. Healthcare providers must exercise caution and consider alternative medications or dosing adjustments to minimize these interactions.
While the potential for interactions between these medications exists, it is crucial not to dismiss their combined use outright. In many cases, the benefits of treating heart conditions with amiodarone or verapamil outweigh the risks associated with statin interactions. Healthcare professionals play a critical role in carefully assessing each patient’s unique situation, carefully selecting the appropriate medications, and closely monitoring for any adverse effects.
Patients prescribed both statins and drugs like amiodarone or verapamil should maintain open and transparent communication with their healthcare providers. Regular check-ups and blood tests can help identify any emerging issues, allowing for prompt adjustments to medication regimens if necessary. Ultimately, the goal is to strike a balance between managing heart conditions effectively and minimizing the potential for side effects, ensuring that patients receive the best possible care for their overall cardiovascular health.
You can also read more about this here: Grapefruit Juice and Some Drugs Don’t Mix | FDA
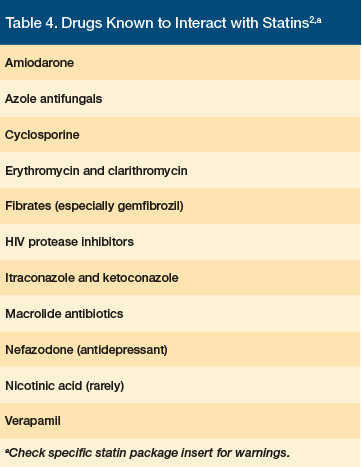
Fibrates, another class of cholesterol-lowering medications, can interact with statins, potentially increasing the risk of muscle-related side effects.
Fibrates, while effective in their own right as cholesterol-lowering medications, introduce a noteworthy element of complexity when used in conjunction with statins. These two classes of drugs, though capable of individually managing cholesterol levels, have the potential to interact in ways that warrant careful consideration, especially in terms of muscle-related side effects.
Fibrates primarily target triglycerides and can be particularly beneficial for individuals with high triglyceride levels. They work by enhancing the breakdown of these fats in the bloodstream, reducing their concentration and lowering the risk of heart disease. However, when fibrates and statins are combined, there’s a heightened concern regarding the muscles, as both medications can independently increase the risk of muscle-related complications.
This interaction between fibrates and statins can lead to a condition known as rhabdomyolysis, a rare but serious condition where muscle tissue breaks down and releases a protein called myoglobin into the bloodstream. Myoglobin can be harmful to the kidneys, potentially causing kidney damage. Although such severe cases are infrequent, it underscores the importance of close monitoring when using both classes of medications together.
Healthcare providers carefully assess the benefits versus risks of combining fibrates with statins, taking into account individual patient profiles and cholesterol levels. If this combination is deemed necessary, vigilant monitoring becomes crucial. Patients prescribed both medications should report any unusual muscle pain, weakness, or tenderness promptly, as these could be early signs of muscle-related side effects. In such cases, adjusting the medication regimen or discontinuing one of the drugs may be necessary to ensure patient safety.
It’s worth noting that while the interaction between fibrates and statins can pose challenges, it can also be a valuable therapeutic option for individuals with complex cholesterol management needs. The decision to combine these medications should always be made in consultation with a healthcare provider who can weigh the potential benefits against the risks and tailor the treatment plan to best address each patient’s unique health circumstances.
In essence, the interaction between fibrates and statins shines a light on the intricate balancing act required in managing cholesterol levels and underscores the importance of informed medical guidance to ensure the best outcomes for patients seeking to optimize their cardiovascular health.
Don’t stop here; you can continue your exploration by following this link for more details: Recommendations for Management of Clinically Significant Drug …
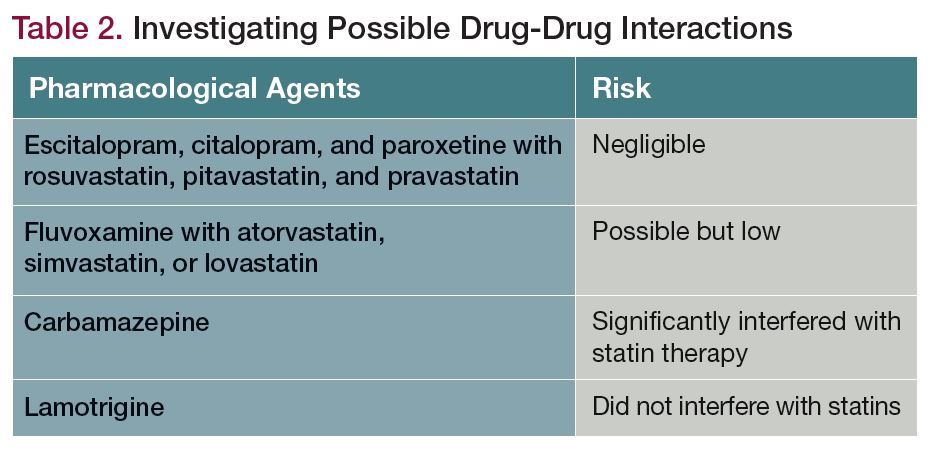
Medications used to suppress the immune system, such as cyclosporine, can interact with statins, leading to higher statin levels in the bloodstream.
The intricate dance between medications within our bodies often results in unexpected interactions, and one such interaction of concern occurs when medications used to suppress the immune system cross paths with statins. One prominent example is cyclosporine, a medication prescribed to prevent organ rejection in transplant patients and manage certain autoimmune conditions.
The interaction between cyclosporine and statins can have significant implications for an individual’s health. When these two medications are used concurrently, the levels of statins in the bloodstream can surge. This elevation may amplify the therapeutic effects of statins but also increases the risk of potential side effects, including muscle-related issues.
This interaction underscores the importance of close medical supervision and communication between healthcare providers when managing complex health conditions. It’s vital for patients to inform their healthcare team about all the medications they are taking, both prescription and over-the-counter, to ensure a comprehensive understanding of potential interactions and to tailor treatment plans accordingly.
Moreover, it highlights the need for personalized medicine, where treatment decisions are based on an individual’s unique health profile, including their specific medications and health conditions. In cases where an interaction is identified, alternative medications or adjusted dosages may be considered to maintain the delicate balance between managing one’s health condition and mitigating potential risks.
Ultimately, understanding and managing drug interactions like the one between cyclosporine and statins is essential for patient safety and effective medical treatment. It emphasizes the critical role of healthcare providers in guiding patients through the complexities of medication management and underscores the need for ongoing communication and collaboration in healthcare decision-making.
Don’t stop here; you can continue your exploration by following this link for more details: Grapefruit–medication interactions: Forbidden fruit or avoidable …

Always inform your healthcare provider about all medications, supplements, and over-the-counter drugs you are taking. They can assess potential interactions and adjust your treatment plan accordingly.
Always inform your healthcare provider about all medications, supplements, and over-the-counter drugs you are taking. This open communication is not just a precautionary measure; it’s a fundamental aspect of responsible healthcare management.
By providing your healthcare provider with a comprehensive list of everything you’re taking, you empower them to make informed decisions about your treatment plan. This includes assessing potential interactions between different medications or supplements, which can be crucial in preventing adverse effects or ensuring that each component of your regimen works harmoniously.
Moreover, your healthcare provider can also evaluate the necessity and effectiveness of each medication or supplement, ensuring that you’re not taking anything that may be redundant or unnecessary. This can help streamline your treatment plan, potentially reducing the number of medications you need to take and minimizing the risk of overmedication.
Additionally, disclosing all substances you’re using allows your healthcare provider to consider any potential side effects or contraindications. For example, certain medications or supplements may exacerbate underlying medical conditions or counteract the effects of others. Being transparent about your healthcare regimen enables your provider to tailor their recommendations to your specific needs, ensuring that you receive the most effective and safe care possible.
Remember that your healthcare provider is your partner in managing your health, and they are there to provide guidance and support. With complete and accurate information about your medication and supplement use, you both can work together to make informed decisions that prioritize your well-being and optimize your treatment outcomes. So, make it a habit to keep your healthcare provider in the loop about everything you’re taking, no matter how seemingly insignificant, to ensure the best possible care.
To delve further into this matter, we encourage you to check out the additional resources provided here: Paxlovid Drug-Drug Interactions | COVID-19 Treatment Guidelines

In some cases, your doctor may recommend alternative medications with fewer interactions or lower potential for side effects.
In situations where the interaction between statins and another medication poses a significant concern, your healthcare provider may suggest alternative approaches to managing your cholesterol levels while minimizing the risk of adverse effects. Here are some strategies and alternatives your doctor might recommend:
1. Switching to a Different Statin: Not all statins interact with other medications to the same extent. Your doctor may consider switching you to a different statin that has a lower potential for interactions. For example, if you were taking simvastatin, they might switch you to rosuvastatin, which generally has fewer interactions.
2. Combination Medications: In some cases, your healthcare provider might prescribe combination medications that include both a statin and another cholesterol-lowering drug. These combinations are designed to be more convenient and may reduce the need for multiple medications with the associated risks of interactions.
3. Non-Statin Cholesterol Medications: There are several non-statin medications available for managing cholesterol, such as ezetimibe and PCSK9 inhibitors. These drugs work differently from statins and may be a suitable alternative or addition to your treatment plan without the same interaction concerns.
4. Lifestyle Modifications: Lifestyle changes play a significant role in managing cholesterol levels. Your healthcare provider may emphasize the importance of dietary adjustments, regular exercise, and weight management as part of your treatment plan. These lifestyle modifications can complement or even replace the need for medication in some cases.
5. Timing and Monitoring: Sometimes, simply adjusting the timing of when you take your medications can help reduce interactions. Your healthcare provider may recommend taking one medication in the morning and the other in the evening to minimize overlap.
6. Monitoring and Dose Adjustments: Close monitoring of your cholesterol levels and potential side effects is essential when managing interactions. Your healthcare provider may need to adjust the dosages of one or both medications to ensure they are effective and well-tolerated without causing complications.
7. Communication and Medication Reconciliation: It’s crucial to maintain open and honest communication with your healthcare team about any changes in your medications or any new supplements you decide to take. Regular medication reconciliation can help ensure that your treatment plan remains safe and effective.
It’s important to remember that the decision to switch or modify your medication regimen should always be made in consultation with your healthcare provider. They will consider your overall health, specific cholesterol goals, and potential interactions when determining the best approach to manage your cholesterol levels effectively while minimizing risks. Your active involvement in discussions about your treatment plan is essential for achieving optimal results in your cholesterol management journey.
Should you desire more in-depth information, it’s available for your perusal on this page: Grapefruit–medication interactions: Forbidden fruit or avoidable …
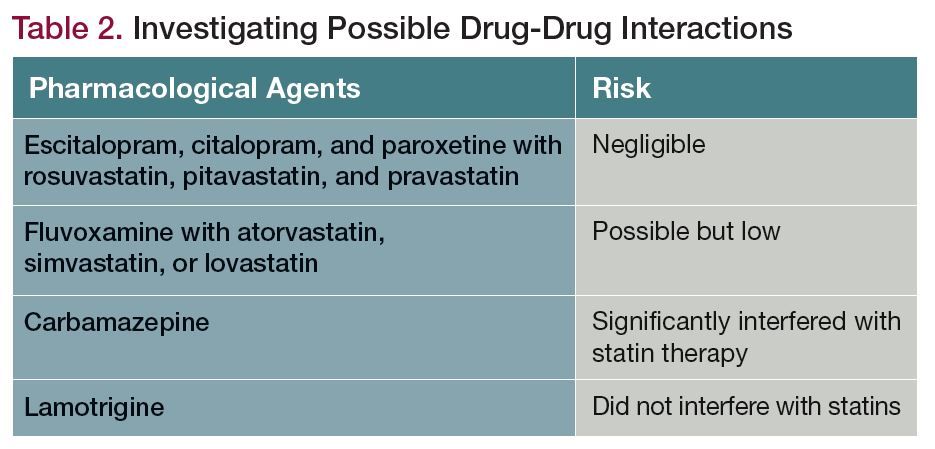
Your healthcare provider may adjust the dosage of your statin or the interacting medication to minimize the risk of adverse effects.
Your healthcare provider’s expertise in managing your medication regimen is invaluable, especially when it comes to statins and their potential interactions with other drugs. When faced with a situation where you’re prescribed both a statin and another medication, your doctor may make dosage adjustments to strike a delicate balance between effectively lowering cholesterol and minimizing the risk of adverse effects.
One common scenario is when your healthcare provider prescribes a medication known to interact with statins. This interaction can sometimes affect how your body processes the statin, potentially leading to an increased risk of side effects or complications. To address this, your doctor may consider adjusting the dosage of either the statin or the interacting medication.
For instance, if you’re taking a medication that has the potential to increase the concentration of statins in your bloodstream, your doctor may reduce the statin dosage to prevent it from reaching levels that could lead to side effects. Conversely, if you’re on a medication that might decrease the effectiveness of the statin, your doctor may opt to increase the statin dosage to maintain its cholesterol-lowering benefits.
These dosage adjustments are part of a careful, personalized approach to ensure that you receive the most effective and safe treatment. It’s crucial to maintain open communication with your healthcare provider throughout this process. They will monitor your progress, conduct regular check-ups, and may order blood tests to assess how your body is responding to the medications.
It’s also essential to inform your healthcare provider about any changes in your overall health or any new medications you might be taking, even if they are over-the-counter or herbal supplements. This information allows your doctor to make informed decisions about dosage adjustments and any necessary modifications to your treatment plan.
Remember that the goal of these adjustments is to optimize the benefits of statin therapy while minimizing the risk of adverse effects or interactions with other medications. By working closely with your healthcare provider and following their guidance, you can confidently manage your cholesterol levels and overall health while keeping potential medication-related issues at bay.
You can also read more about this here: AHA Statement on Drug-Drug Interactions With Statins – American …
Regular monitoring, including blood tests to assess liver function and muscle enzymes, can help detect any issues related to drug interactions early on.
Regular monitoring of your health is a crucial component of safe and effective medication management, particularly when it comes to medications like statins that may have potential side effects. This proactive approach, which often includes blood tests to assess liver function and muscle enzymes, serves as a valuable tool in identifying and addressing any issues related to drug interactions before they escalate.
1. Liver Function: Statins are primarily metabolized by the liver, which means this vital organ plays a significant role in how these medications are processed in your body. Regular monitoring of liver function through blood tests allows healthcare providers to detect any abnormalities or signs of liver stress early on. While liver issues related to statins are relatively rare, prompt identification can help prevent serious complications.
2. Muscle Enzymes: One of the more commonly known side effects of statins is muscle-related symptoms, ranging from mild discomfort to a rare but serious condition called rhabdomyolysis. Elevated muscle enzymes in the bloodstream can be an early indicator of muscle-related issues. Regular testing enables your healthcare provider to assess whether these enzymes are within a healthy range or if further investigation and potential adjustments to your medication are necessary.
3. Individualized Care: Regular monitoring goes hand in hand with personalized care. Each person’s response to medication can vary, and by closely tracking your health parameters, your healthcare provider can tailor your treatment plan to your specific needs. They can also make informed decisions about dosage adjustments, medication changes, or the inclusion of other interventions to ensure your health and well-being.
4. Preventive Approach: Regular monitoring isn’t just about addressing issues as they arise; it’s also a preventive measure. By proactively assessing your health, your healthcare provider can identify potential concerns before they become serious. This approach aligns with the principle of minimizing risks associated with medication use, ultimately helping you enjoy the benefits of treatment with greater peace of mind.
5. Patient Education: In addition to the clinical aspects, regular monitoring provides an opportunity for patient education. Your healthcare provider can engage in meaningful discussions with you about your medication, potential side effects, and strategies for managing your health. This dialogue empowers you to take an active role in your well-being and make informed decisions about your treatment.
In conclusion, regular monitoring, including blood tests to assess liver function and muscle enzymes, is a proactive and essential component of medication management, especially when taking statins or any medication with potential side effects. It helps ensure your health and safety while on medication and allows for individualized care that addresses your specific needs. Embrace this monitoring as a valuable tool on your journey to better health, and maintain open communication with your healthcare provider to make the most of this comprehensive approach to care.
Should you desire more in-depth information, it’s available for your perusal on this page: Drug Interactions with Lithium and Therapeutic Drug Monitoring
Alongside medication management, lifestyle changes such as a heart-healthy diet and regular exercise can play a crucial role in managing cholesterol levels.
Alongside medication management, lifestyle changes such as adopting a heart-healthy diet and incorporating regular exercise into your daily routine can play a pivotal and empowering role in managing cholesterol levels and overall cardiovascular health.
Dietary Wisdom: Embracing a heart-healthy diet involves making thoughtful choices that prioritize foods known to benefit your heart. Incorporate a variety of nutrient-rich foods like fruits, vegetables, whole grains, and lean proteins into your meals. Opt for unsaturated fats found in sources like olive oil, avocados, and nuts, while minimizing saturated and trans fats. Foods rich in soluble fiber, such as oats, beans, and lentils, can actively help lower LDL (“bad”) cholesterol levels. And don’t forget the power of omega-3 fatty acids, found in fatty fish like salmon and mackerel, for reducing triglycerides and supporting heart health.
Exercise as Medicine: Regular physical activity is a potent tool for managing cholesterol levels and promoting overall cardiovascular wellness. Engaging in activities like brisk walking, jogging, cycling, or swimming can boost your HDL (“good”) cholesterol while helping to lower LDL cholesterol and triglycerides. Exercise also enhances your body’s sensitivity to insulin, assists in weight management, and strengthens your heart, all of which contribute to better cholesterol control.
Weight Management: Maintaining a healthy weight is closely linked to cholesterol management. Shedding excess pounds, even a modest amount, can lead to improvements in cholesterol profiles. Combined with a balanced diet and exercise regimen, weight management can help optimize your lipid levels and reduce the risk of cardiovascular disease.
Stress Reduction: Chronic stress can impact cholesterol levels and heart health. Practicing stress management techniques such as mindfulness, meditation, yoga, or deep breathing exercises can help lower stress hormones and contribute to healthier cholesterol profiles.
Smoking Cessation: Smoking not only negatively affects cholesterol levels but also significantly raises the risk of heart disease. Quitting smoking is one of the most powerful steps you can take to improve your overall cardiovascular health.
Regular Monitoring: Regular check-ups with your healthcare provider are crucial to monitor your cholesterol levels and assess your overall cardiovascular risk. These appointments allow for adjustments in your medication, diet, or exercise plan as needed to achieve and maintain optimal lipid profiles.
By integrating these lifestyle changes into your daily routine, you become an active participant in managing your cholesterol levels and supporting your heart health. While medication remains an essential component of treatment for many individuals, these non-pharmacological approaches are both complementary and empowering, providing you with the tools to take charge of your cardiovascular well-being and enjoy a heart-healthy life.
For additional details, consider exploring the related content available here Management of dyslipidemia in HIV-infected patients – PMC
Conclusion
Statin drug interactions can be a concern, but with proper awareness and communication with your healthcare provider, they can be managed effectively. It’s crucial to understand that not all interactions lead to problems, and many individuals can safely take statins alongside other medications.
The key is to stay informed, communicate openly with your healthcare team, and follow their guidance closely. By doing so, you can reap the benefits of statins while minimizing the risks associated with potential drug interactions, ultimately working toward better heart health and a reduced risk of cardiovascular disease.
Statin drug interactions are a legitimate concern for those managing their cholesterol levels, but there’s no need to let anxiety overshadow their benefits. With proper awareness and open communication with your healthcare provider, these interactions can be managed effectively, allowing you to maintain optimal heart health.
First and foremost, it’s essential to recognize that not all interactions pose a threat to your well-being. Many individuals safely combine statins with other medications without any issues. The key to success lies in staying well-informed about your medications, sharing your complete medical history with your healthcare team, and following their guidance meticulously.
Regular check-ins with your healthcare provider are an opportunity to discuss any concerns, review your medication regimen, and make adjustments if necessary. They can help identify potential interactions and find suitable solutions, whether it involves adjusting dosages, changing medications, or monitoring your progress more closely.
By taking an active role in your healthcare, you can reap the benefits of statins while minimizing the risks associated with potential drug interactions. This proactive approach not only promotes better heart health but also provides peace of mind, knowing that you’re working collaboratively with your healthcare team to reduce the risk of cardiovascular disease and improve your overall well-being. Remember, your health is a partnership, and open communication is the key to its success.
To expand your knowledge on this subject, make sure to read on at this location: Clinical Data Repositories: Primary Sources of Drug-to-Drug …
More links
Looking for more insights? You’ll find them right here in our extended coverage: Statin side effects: Weigh the benefits and risks – Mayo Clinic
