Introduction
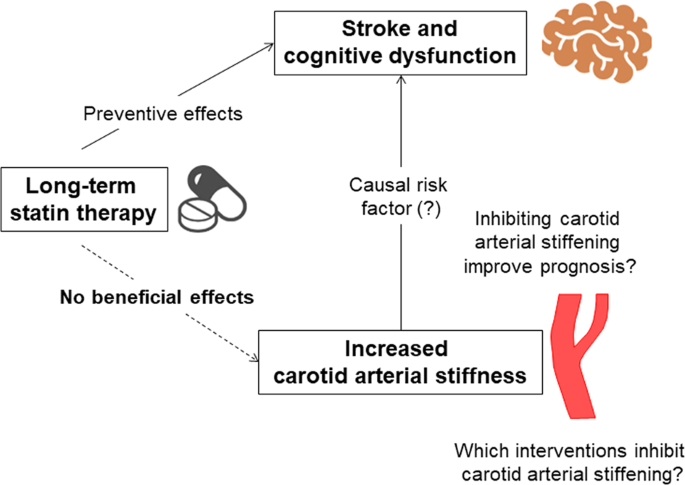
Statins have long been regarded as a cornerstone in the prevention and management of cardiovascular diseases. These cholesterol-lowering medications have saved countless lives by reducing the risk of heart attacks, strokes, and other cardiovascular events. However, recent advancements in medical research have highlighted the significance of genetic predisposition in determining an individual’s response to statin therapy. This discovery has opened up new avenues for tailoring treatment to accommodate genetic variants, thereby optimizing the benefits of statin therapy.
Statins have held a well-deserved place as a cornerstone in the prevention and management of cardiovascular diseases for quite some time. These cholesterol-lowering medications have been nothing short of lifesavers, contributing significantly to the reduction of heart attacks, strokes, and other cardiovascular events worldwide. However, the landscape of statin therapy is evolving, thanks to recent advancements in medical research that have shed light on the vital role of genetic predisposition in an individual’s response to these medications. This groundbreaking discovery has ushered in a new era of personalized medicine, offering the potential to optimize the benefits of statin therapy in an even more precise and tailored manner.
The Power of Genetic Insights: Understanding genetic predisposition in the context of statin therapy is like uncovering a missing puzzle piece. It allows healthcare providers to peer into an individual’s unique genetic makeup and predict how they might respond to statins. Some genetic variants, for instance, influence how the body metabolizes statins, impacting their effectiveness and potential side effects.
Personalized Treatment Plans: Armed with this genetic information, healthcare providers can craft personalized treatment plans. They can select the most suitable statin type and dosage for each patient, optimizing the likelihood of a favorable response and minimizing the risk of adverse effects. This tailoring approach holds the promise of enhancing both the effectiveness and tolerability of statin therapy.
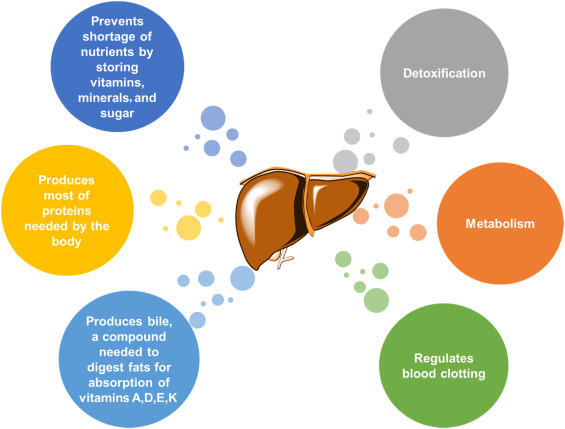
Mitigating Side Effects: Statin-related side effects, such as muscle pain or liver abnormalities, can deter some individuals from adhering to their prescribed treatment. Genetic insights can help identify individuals at higher risk of these side effects, enabling proactive monitoring and adjustments to minimize discomfort or risks.
Reducing Cardiovascular Risk: Beyond the immediate benefits of optimized statin therapy, the integration of genetic information into treatment decisions has the potential to further reduce cardiovascular risk. By tailoring therapy to an individual’s genetic profile, healthcare providers can enhance the overall impact on cholesterol levels and, consequently, on the reduction of heart disease risk.
Shared Decision-Making: Incorporating genetics into statin therapy fosters a collaborative approach to healthcare. It empowers patients with a deeper understanding of their own genetic risk factors and treatment options, enabling them to make more informed decisions in partnership with their healthcare providers.
The Road Ahead: While the integration of genetics into statin therapy is a promising development, it’s worth noting that it’s still an evolving field. Continued research is essential to refine our understanding of how genetic factors influence statin response and to identify additional genetic markers. Furthermore, the cost-effectiveness and accessibility of genetic testing are areas of ongoing exploration.
In conclusion, the recognition of genetic predisposition as a crucial factor in statin therapy represents a significant stride towards personalized medicine in the realm of cardiovascular health. This discovery not only underscores the importance of individualized care but also opens up exciting possibilities for tailoring statin treatment to maximize its benefits while minimizing potential risks. As our understanding of the interplay between genetics and statin therapy deepens, we move closer to a future where heart disease prevention and management are even more finely tuned to the unique needs of each patient.
If you’d like to dive deeper into this subject, there’s more to discover on this page: Pharmacogenetics: An Important Part of Drug Development with A …
Statins are a class of drugs primarily prescribed to lower cholesterol levels in the bloodstream. They work by inhibiting the enzyme responsible for cholesterol production in the liver, ultimately reducing the amount of cholesterol circulating in the blood. Lowering cholesterol levels is essential because high cholesterol is a well-established risk factor for atherosclerosis, the buildup of fatty plaques in the arteries that can lead to heart disease.
Statins have proven to be highly effective in reducing cholesterol levels and, consequently, lowering the risk of cardiovascular events. They are often prescribed to individuals with high cholesterol, a history of heart disease, or those at an elevated risk of developing cardiovascular problems.
Additionally, you can find further information on this topic by visiting this page: Pharmacogenomics of statins: understanding susceptibility to …

While statins are generally effective, not everyone responds to them in the same way. Some individuals experience significant reductions in cholesterol levels and a lowered risk of cardiovascular events when taking statins, while others may not derive the same benefits. This discrepancy in response has led researchers to explore the role of genetics in determining how individuals metabolize and respond to statins.
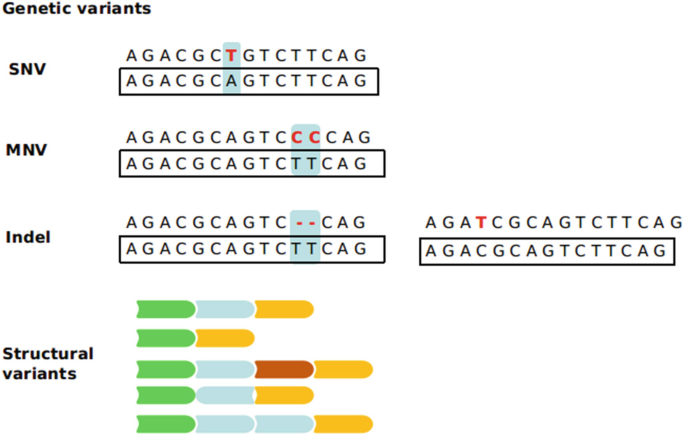
Several genetic variants have been identified that can influence an individual’s response to statin therapy. One of the most well-known genetic variants is in the gene encoding for the enzyme cytochrome P450 3A4 (CYP3A4). This enzyme plays a crucial role in metabolizing statins. Genetic variations in CYP3A4 can affect how efficiently an individual’s body processes statins, potentially leading to variations in drug efficacy and side effects.
Another genetic factor to consider is the presence of specific polymorphisms in the SLCO1B1 gene, which codes for a protein responsible for transporting statins into the liver. Variations in this gene can impact the uptake of statins, influencing their effectiveness and the risk of adverse effects.
To delve further into this matter, we encourage you to check out the additional resources provided here: Pharmacogenomics of statins: understanding susceptibility to …
The recognition of genetic variants influencing statin response has paved the way for personalized medicine in cardiovascular care. Tailoring statin treatment to an individual’s genetic makeup has the potential to maximize the benefits of therapy while minimizing side effects.
Here are some key steps in tailoring statin treatment based on genetic predisposition:
The emergence of genetic variants that influence an individual’s response to statin therapy has opened up exciting possibilities for personalized medicine in the realm of cardiovascular care. This approach acknowledges the unique genetic makeup of each patient, allowing for the customization of statin treatment to maximize its benefits while minimizing the risk of side effects. Here are some essential steps in tailoring statin treatment based on genetic predisposition:
Genetic Testing: The journey towards personalized statin therapy begins with genetic testing. Specific genetic tests can identify variations in genes related to statin metabolism and cholesterol regulation. This information provides valuable insights into how an individual may respond to statin treatment.
Risk Assessment: Genetic testing results should be considered alongside other risk factors, such as age, family history, and existing health conditions. This comprehensive assessment helps healthcare providers determine the patient’s overall cardiovascular risk and informs the decision-making process.
Choosing the Right Statin: Based on genetic and clinical information, healthcare providers can select the most appropriate statin medication for the individual. Some statins may be better suited for certain genetic profiles, offering a higher likelihood of efficacy and fewer side effects.
Optimal Dosage: Personalized medicine allows for the precise adjustment of statin dosage. Genetic information can guide healthcare providers in determining the most effective dose for cholesterol control while minimizing the risk of side effects.
Monitoring and Adjustments: Regular monitoring of cholesterol levels and overall health is crucial in personalized statin therapy. It enables healthcare providers to assess treatment efficacy and make necessary adjustments over time. Monitoring may also include checking for any potential side effects.
Patient Education and Engagement: Patients play an active role in their personalized statin therapy. Understanding their genetic predisposition and the rationale behind treatment decisions empowers individuals to make informed choices and adhere to their medication regimen.
Shared Decision-Making: As with any medical treatment, shared decision-making between healthcare providers and patients is paramount. Open and collaborative discussions ensure that treatment plans align with the patient’s preferences, values, and goals for cardiovascular health.
Lifestyle Factors: While genetic predisposition is a significant consideration, lifestyle factors such as diet, physical activity, and smoking status continue to exert a profound influence on cardiovascular health. Integrating lifestyle modifications into personalized statin therapy can amplify the benefits of treatment.
In conclusion, the era of personalized medicine in cardiovascular care represents a promising frontier for optimizing statin therapy. By harnessing the power of genetic information and combining it with a holistic approach to patient care, healthcare providers can tailor statin treatment to each individual’s unique genetic makeup and overall health profile. This personalized approach not only enhances the effectiveness of statin therapy but also promotes patient engagement and satisfaction, fostering a more precise and patient-centered approach to cardiovascular care.
Don’t stop here; you can continue your exploration by following this link for more details: Pharmacogenetics: An Important Part of Drug Development with A …
Before initiating statin therapy, individuals can undergo genetic testing to identify any relevant genetic variants. This information can help healthcare providers make informed decisions about the choice of statin, dosage, and monitoring.
Before initiating statin therapy, individuals can undergo genetic testing to identify any relevant genetic variants. This information can significantly enhance the precision of statin treatment in several ways:
Personalized Medication Selection: Genetic testing can reveal how an individual’s genes affect their response to statins. Some genetic variations may make certain statins more effective or better tolerated. Armed with this knowledge, healthcare providers can select the most suitable statin drug for the patient’s unique genetic profile.
Optimal Dosage Determination: Genetic testing can help determine the appropriate statin dosage for an individual. Genetic factors may influence how quickly a person metabolizes the medication, affecting the required dosage for desired cholesterol management without excessive side effects.
Risk Assessment: Genetic testing can identify genetic variants associated with an increased risk of statin-related side effects, such as muscle pain or myopathy. This knowledge allows healthcare providers to closely monitor individuals at higher risk and make timely adjustments to prevent complications.
Treatment Personalization: By tailoring statin therapy based on genetic information, healthcare providers can provide a more personalized approach to cholesterol management. This approach aims to optimize treatment efficacy while minimizing potential side effects.
Improved Adherence: When patients experience fewer side effects and observe better results with a genetically guided statin therapy, they are more likely to adhere to their treatment plan. Enhanced adherence contributes to better long-term cholesterol management and cardiovascular health.
Reduced Trial and Error: Genetic testing can help avoid the trial-and-error approach often associated with finding the right statin and dosage. This can save time and resources while minimizing patient frustration.
Risk Mitigation: Identifying individuals at higher risk of statin-related side effects allows for proactive management. For example, in some cases, healthcare providers may recommend specific supplements or lifestyle modifications to mitigate potential issues.
Patient Empowerment: Genetic testing empowers patients by providing them with valuable information about how their body may respond to statin therapy. This knowledge can lead to more informed discussions and shared decision-making with their healthcare provider.
Future Considerations: Genetic testing may also reveal insights into other aspects of health beyond statin therapy, contributing to a more comprehensive understanding of an individual’s genetic predispositions and health risks.
While genetic testing can enhance the precision of statin therapy, it’s important to note that it is not always necessary for everyone. Its utility may depend on factors such as a person’s medical history, cholesterol levels, and previous experiences with statins. Individuals interested in genetic testing should discuss the option with their healthcare provider to determine its appropriateness and potential benefits for their specific situation.
You can also read more about this here: Genetic variation in human drug-related genes | Genome Medicine …
Depending on an individual’s genetic profile, certain statins may be more suitable than others. For instance, individuals with specific genetic variants may benefit more from pravastatin or rosuvastatin rather than atorvastatin.
The role of genetics in statin therapy is a fascinating area of research that has brought about a deeper understanding of how individuals can respond differently to these medications. Depending on an individual’s genetic profile, certain statins may indeed be more suitable and effective for their specific needs.
Genetic variations can influence how the body metabolizes and interacts with statins. For example, some individuals may possess genetic variants that make them more responsive to pravastatin, while others might see better results with rosuvastatin or another statin option. This genetic variability can extend to both the effectiveness and potential side effects of statin therapy.
For those individuals with a genetic predisposition to metabolize statins at a slower rate, which can increase the risk of side effects, healthcare providers may consider prescribing lower doses or less potent statins. This approach allows patients to achieve the desired cholesterol-lowering effects with reduced potential for adverse reactions.
Conversely, some individuals may have genetic traits that enable them to tolerate higher doses of statins without encountering side effects, making more potent statins like rosuvastatin or atorvastatin a suitable choice for them.
Pharmacogenetic testing has emerged as a valuable tool in helping healthcare providers make informed decisions about statin therapy. This type of testing examines a patient’s genetic makeup to identify variants that can impact statin metabolism and effectiveness. Armed with this information, healthcare providers can personalize statin therapy, choosing the most appropriate statin and dosage for each patient based on their genetic profile.
However, it’s important to note that while pharmacogenetic testing can provide valuable insights, it is just one part of the decision-making process. Healthcare providers consider a range of factors when prescribing statins, including an individual’s overall cardiovascular risk, existing medical conditions, lifestyle, and medication interactions.
Moreover, the field of pharmacogenetics is continually evolving, and ongoing research may uncover new genetic markers and insights into statin therapy. Therefore, individuals interested in exploring pharmacogenetic testing as part of their statin management should discuss it with their healthcare provider, who can provide guidance on the most appropriate approach based on the latest research and clinical guidelines.
In summary, the integration of genetics into statin therapy represents an exciting frontier in personalized medicine. By tailoring statin choices to an individual’s genetic profile, healthcare providers can optimize treatment effectiveness while minimizing potential side effects, ultimately enhancing the management of cholesterol levels and reducing the risk of cardiovascular events.
For a comprehensive look at this subject, we invite you to read more on this dedicated page: Table of Pharmacogenetic Associations | FDA

Genetic information can also guide dosage adjustments. Some individuals may require lower or higher doses of statins to achieve the desired cholesterol-lowering effect while minimizing side effects.
Genetic information is a powerful tool in the realm of healthcare, and it can significantly enhance the precision and effectiveness of statin therapy. Beyond aiding in the selection of the most appropriate statin for an individual, genetic data can also provide crucial insights for dosage adjustments.
The way our bodies metabolize medications, including statins, can be influenced by our genetic makeup. Some individuals may have genetic variations that affect how quickly or slowly they process these drugs. As a result, they may require lower or higher doses of statins to achieve the desired cholesterol-lowering effect while minimizing side effects.
For those who metabolize statins more slowly, lower doses may be sufficient to achieve optimal results without an increased risk of side effects. On the other hand, individuals who metabolize statins quickly may require higher doses to achieve the same cholesterol-lowering effect.
Genetic testing can identify these metabolic variations, enabling healthcare providers to tailor statin dosages to an individual’s unique genetic profile. This personalized approach not only maximizes the effectiveness of the medication but also minimizes the risk of side effects, ultimately enhancing the overall treatment experience.
Moreover, genetic information can provide insights into the likelihood of specific side effects, such as muscle-related issues. Some genetic markers are associated with an increased susceptibility to statin-induced muscle problems. By identifying these markers, healthcare providers can proactively monitor for potential side effects and adjust treatment plans accordingly.
Incorporating genetic information into statin therapy exemplifies the concept of personalized medicine. It acknowledges that individuals have distinct responses to medications based on their genetic characteristics. By tailoring statin dosages and monitoring plans to align with these unique traits, healthcare providers can optimize the benefits of cholesterol management while minimizing potential drawbacks.
It’s important to note that genetic testing for statin therapy is not yet standard practice in all healthcare settings. However, its use is growing, and it holds great promise for improving the precision and safety of statin treatment. As genetic research continues to advance, we can anticipate even more refined approaches to individualizing statin therapy, further enhancing its effectiveness and patient satisfaction.
You can also read more about this here: Genetic variation in human drug-related genes | Genome Medicine …
Regular monitoring of cholesterol levels and any potential side effects is crucial. Genetic factors may influence how often and intensively monitoring is required.
In the realm of cholesterol management, consistent monitoring is not merely advisable; it’s a fundamental element of maintaining heart health. Regularly tracking your cholesterol levels and staying vigilant about potential side effects is a proactive approach that can make a significant difference in your well-being.
However, it’s important to recognize that the frequency and intensity of monitoring may not be a one-size-fits-all scenario. Genetic factors can exert a substantial influence on an individual’s cholesterol profile and how their body responds to cholesterol-lowering interventions.
For some, genetic predispositions may lead to more stubbornly elevated cholesterol levels, necessitating closer and more frequent monitoring to ensure that treatment plans remain effective. In such cases, healthcare providers may recommend more frequent blood tests to assess cholesterol levels and adjust treatment strategies accordingly.
Conversely, individuals with a more favorable genetic makeup may respond well to cholesterol-lowering interventions, requiring less intensive monitoring. Nevertheless, regular check-ups remain essential to ensure that cholesterol levels remain within a healthy range and to promptly detect any potential side effects associated with medications like statins.
Furthermore, the landscape of cholesterol management is continually evolving. Research advances and the development of new medications mean that healthcare providers have a broader array of options to tailor treatment plans to individual needs. Genetic testing can sometimes provide valuable insights into how a person’s genetic makeup may influence their response to specific cholesterol-lowering medications, helping healthcare providers make more informed decisions about the most effective and suitable treatments.
In conclusion, while regular monitoring of cholesterol levels and potential side effects is universally important, the approach should be individualized to accommodate genetic factors and personal health considerations. This personalized approach ensures that cholesterol management is not a one-time decision but a dynamic and evolving process that adapts to the unique needs of each individual, ultimately promoting better heart health and overall well-being.
Additionally, you can find further information on this topic by visiting this page: Personalized sequencing and the future of medicine: discovery …
In addition to statin therapy, individuals should continue with lifestyle modifications, such as a heart-healthy diet, regular exercise, and smoking cessation, to further reduce cardiovascular risk.
In the quest for optimal heart health, the role of lifestyle modifications cannot be overstated. While statin therapy is a valuable tool in managing cholesterol levels and reducing cardiovascular risk, it is most effective when complemented by a comprehensive approach that encompasses heart-healthy habits and choices.
First and foremost, maintaining a heart-healthy diet is a cornerstone of cardiovascular well-being. This means emphasizing a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats while minimizing saturated and trans fats, added sugars, and excessive salt. Such a diet can help lower cholesterol levels, reduce blood pressure, and maintain a healthy weight, all of which are crucial factors in heart disease prevention.
Regular exercise is another vital component of a heart-healthy lifestyle. Physical activity strengthens the heart muscle, improves blood vessel function, and helps control weight. Moreover, it contributes to the management of other risk factors such as diabetes and high blood pressure. Engaging in moderate-intensity exercise, like brisk walking, swimming, or cycling, for at least 150 minutes per week is recommended to reap these cardiovascular benefits.
One of the most impactful choices an individual can make for their heart health is to quit smoking. Smoking is a major risk factor for heart disease, as it damages blood vessels, increases blood pressure, and decreases the level of “good” HDL cholesterol. Quitting smoking not only lowers the risk of heart disease but also leads to significant improvements in overall health. Various resources and support systems are available to aid in smoking cessation, making it an achievable goal for those looking to safeguard their heart health.
Beyond diet, exercise, and smoking cessation, other lifestyle factors can also influence cardiovascular risk. Managing stress through relaxation techniques, mindfulness, or hobbies can contribute to heart health. Getting sufficient sleep is equally important, as poor sleep patterns have been linked to an increased risk of heart disease.
In essence, while statin therapy plays a crucial role in cholesterol management and heart disease prevention, it operates most effectively when integrated into a holistic lifestyle approach. By combining the power of medication with heart-healthy habits like a balanced diet, regular exercise, smoking cessation, stress management, and adequate sleep, individuals can significantly reduce their cardiovascular risk and pave the way for a longer and healthier life. It’s a partnership between medical intervention and personal choices that empowers individuals to take control of their heart health and enjoy the benefits of a strong and resilient cardiovascular system.
Should you desire more in-depth information, it’s available for your perusal on this page: Polygenic risk scores: from research tools to clinical instruments …
Conclusion
The recognition of genetic predisposition in determining an individual’s response to statin therapy represents a significant advancement in cardiovascular medicine. Tailoring statin treatment based on genetic variants can optimize the benefits of these medications while minimizing the risk of adverse effects. As genetic testing becomes more accessible and affordable, personalized statin therapy has the potential to improve the long-term cardiovascular outcomes for many individuals. However, it’s crucial to consult with healthcare professionals who can interpret genetic data and develop individualized treatment plans to ensure the best possible outcomes.
Explore this link for a more extensive examination of the topic: Genetics of Familial Hypercholesterolemia: New Insights – Frontiers
More links
If you’d like to dive deeper into this subject, there’s more to discover on this page: Genetics of Coronary Artery Disease | Circulation Research