Introduction
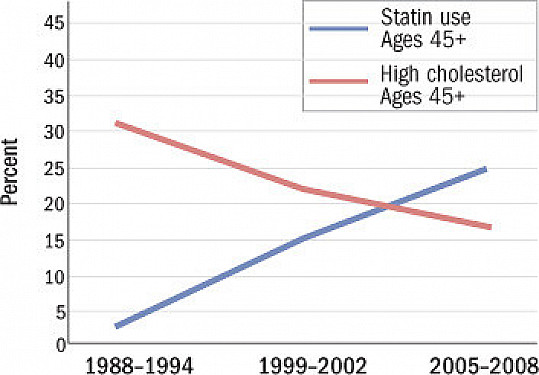
Statin medications have long been a subject of both praise and controversy in the realm of healthcare. While they are widely regarded as effective in lowering cholesterol and reducing cardiovascular risk, statins have also been the center of various myths and concerns. In this article, we will delve into the controversies surrounding statin use, debunk common myths, and provide clarity on their safety and benefits.
The realm of healthcare has witnessed an enduring debate surrounding statin medications, a dialogue that is marked by both praise and controversy. On one hand, statins are hailed as effective tools in the fight against elevated cholesterol levels and the associated cardiovascular risks. On the other hand, they have found themselves at the center of various myths, concerns, and misconceptions. In this article, our aim is to delve deep into the controversies that have enveloped statin use, dispel common myths, and provide the much-needed clarity on their safety and undeniable benefits.
1. Efficacy and Cholesterol Control: Statins have consistently demonstrated their effectiveness in lowering LDL (low-density lipoprotein) cholesterol, often referred to as “bad” cholesterol. This reduction is directly linked to a decreased risk of heart attacks and strokes. Yet, questions and skepticism about their efficacy persist, causing some individuals to doubt their benefits.
2. Safety Concerns: Some have expressed concerns about potential side effects of statins, such as muscle pain and liver enzyme elevations. While these side effects are relatively rare, they have contributed to a degree of apprehension among patients. It’s important to examine the actual risk and how healthcare providers monitor and manage these concerns.
3. Debunking Myths: Statins have faced their fair share of myths, including notions that they cause memory loss, increase the risk of diabetes, or are ineffective in certain populations. We will carefully dissect these myths, relying on scientific evidence to provide clear, evidence-based information.
4. Personalized Care: The controversy surrounding statin use also touches on the need for personalized care. One size does not fit all in medicine, and statin therapy is no exception. We will explore the importance of tailored treatment plans that consider individual factors, such as age, genetics, and existing health conditions.
5. Communicating Benefits: Amidst the controversy, it’s crucial to emphasize the undeniable benefits of statins in preventing cardiovascular events. We will spotlight the positive impact these medications have had on countless lives and underscore their role in enhancing heart health.
In the face of these controversies, our goal is to provide a comprehensive and balanced view of statin medications. By addressing common concerns, debunking myths, and highlighting their proven benefits, we aim to empower individuals to make informed decisions about their health. Ultimately, the goal is to foster a clearer understanding of statins, recognizing them as a valuable tool in the pursuit of cardiovascular well-being while acknowledging the importance of personalized, patient-centered care.
Don’t stop here; you can continue your exploration by following this link for more details: Cardiovascular Disease and the Female Disadvantage – PMC
Before addressing the controversies, it’s essential to understand why statins are prescribed and their proven benefits:
Before delving into the controversies surrounding statin medications, it’s imperative to establish a solid foundation of understanding regarding their prescription and the well-documented benefits they offer. This knowledge forms the basis for informed discussions and decision-making concerning the use of these drugs in managing cardiovascular health.
Primary Role in Cholesterol Management: Statins are primarily prescribed for their remarkable ability to lower cholesterol levels, particularly LDL (“bad”) cholesterol. Elevated LDL cholesterol is a significant risk factor for atherosclerosis, a condition characterized by the buildup of fatty deposits in the arteries, which can lead to heart attacks and strokes. Statins work by inhibiting an enzyme involved in cholesterol production, effectively reducing the amount of cholesterol circulating in the bloodstream.
Proven Cardiovascular Benefits: Decades of clinical research have unequivocally demonstrated the cardiovascular benefits of statins. They have been shown to reduce the risk of heart attacks, strokes, and other cardiovascular events in both individuals with established heart disease and those at risk of developing it. Statins are often prescribed as a preventive measure to lower this risk, especially in individuals with specific risk factors like diabetes or a history of cardiovascular events.
Role in Preventive Medicine: Statins play a crucial role in preventive medicine, and they are recommended as a cornerstone of therapy in various clinical guidelines. Their use in high-risk individuals can significantly improve outcomes, enhance quality of life, and, in many cases, extend life expectancy.
Scientific Consensus: The prescription of statins is firmly grounded in scientific consensus. Their efficacy and safety have been thoroughly evaluated in large-scale clinical trials involving diverse patient populations. These trials consistently demonstrate that the benefits of statin therapy far outweigh any potential risks for most individuals.
Individualized Treatment: It’s important to note that statin therapy is not a one-size-fits-all solution. Healthcare providers prescribe statins based on an individual’s unique medical history, risk factors, and cholesterol levels. The choice of statin, dosage, and duration of treatment is tailored to each patient, ensuring that the benefits align with their specific needs and circumstances.
Adherence to Therapy: Adherence to statin therapy is crucial for achieving optimal results. Patients are encouraged to take their medications as prescribed and maintain open communication with their healthcare providers regarding any concerns or side effects they may experience. In cases of intolerable side effects, healthcare providers can explore alternative treatment options.
In conclusion, understanding the well-established role of statins in managing cholesterol levels and preventing cardiovascular events is essential. Armed with this knowledge, individuals and healthcare providers can make informed decisions about the use of statins, considering their potential benefits and any associated controversies. It is within this informed context that the controversies surrounding statins can be explored and evaluated.
Should you desire more in-depth information, it’s available for your perusal on this page: 3 Myths About Cholesterol-Lowering Statin Drugs | Johns Hopkins …

Now, let’s address some of the common controversies and myths surrounding statin use:
Now, let’s dive into the realm of common controversies and misconceptions that often swirl around the topic of statin use. These debates and myths can create confusion and even deter individuals from pursuing statin therapy when it could be beneficial.
One common controversy revolves around the idea that statins are overprescribed. While there is ongoing discussion about the appropriate criteria for prescribing statins, it’s essential to recognize that they are prescribed based on a careful assessment of individual risk factors and cholesterol levels. Overprescription can be an issue, but it’s equally important not to underprescribe when statins could potentially save lives.
Another myth pertains to the notion that statins are a one-size-fits-all solution. In reality, not everyone benefits equally from these medications, and their effectiveness can vary from person to person. This is why personalized medicine and individualized treatment plans are becoming increasingly important in the field of statin therapy.
Additionally, concerns about statin side effects often emerge as a contentious topic. While statins are generally well-tolerated, some individuals may experience side effects, such as muscle pain. However, these side effects are relatively rare, and healthcare providers can work with patients to find suitable alternatives or solutions.
Lastly, there’s the notion that once you start taking statins, you’re committed for life. While long-term statin therapy is common for many individuals, it’s not necessarily a lifelong commitment for everyone. Treatment duration can vary based on individual needs, and decisions about continuing or discontinuing statin therapy should be made in consultation with a healthcare provider.
By addressing these common controversies and myths, we aim to provide clarity and dispel misconceptions surrounding statin use. It’s essential to approach these discussions with a balanced and evidence-based perspective, ensuring that individuals can make informed decisions about their heart health and well-being.
Don’t stop here; you can continue your exploration by following this link for more details: Myths About Cholesterol, Debunked | Time

While statins can lead to elevated liver enzyme levels in some individuals, serious liver damage due to statin use is rare. Routine monitoring helps detect any abnormalities early.
Statins have become a cornerstone in the management of cholesterol levels and the prevention of heart disease, yet concerns about their impact on liver health persist. It’s important to clarify that while statins can indeed lead to elevated liver enzyme levels in certain individuals, the occurrence of serious liver damage directly caused by statin use is an exceedingly rare occurrence.
These medications have undergone rigorous testing and extensive clinical trials to ensure their safety, and the benefits of lowering cholesterol and reducing the risk of heart attacks and strokes are well-established. Nevertheless, it’s prudent to exercise caution and maintain a proactive approach when using statins, which includes routine monitoring of liver enzyme levels.
Liver enzymes are essential markers of liver function, and they can temporarily increase in response to statin use. This elevation is generally benign and reversible once statin treatment is either adjusted or discontinued. It is often a sign that the liver is adapting to the medication.
Routine monitoring, typically through blood tests, is a crucial part of statin therapy. These tests can identify any concerning changes in liver enzyme levels early, allowing healthcare providers to take appropriate action. Most individuals who experience mild increases in liver enzyme levels can continue to benefit from statin therapy by either adjusting the dosage or switching to a different statin, which may be better tolerated.
It’s vital to emphasize that the risk of serious liver damage directly attributable to statins is exceptionally low. For the vast majority of people, the benefits of these medications in preventing heart disease far outweigh the minimal risk associated with liver enzyme elevation. However, open communication with your healthcare provider is essential. If you have any concerns or experience unusual symptoms while on statins, such as unexplained fatigue, jaundice, or abdominal discomfort, these should be promptly reported to your healthcare provider for evaluation.
In conclusion, while the potential for statins to elevate liver enzyme levels exists, the risk of serious liver damage from statin use is exceedingly rare. Routine monitoring of liver enzyme levels is a proactive measure to ensure early detection and appropriate management of any abnormalities. The safety profile of statins, coupled with their well-documented cardiovascular benefits, underscores their importance in the arsenal of treatments for individuals striving to maintain heart health.
To expand your knowledge on this subject, make sure to read on at this location: Myths About Cholesterol, Debunked | Time

Myopathy is a potential side effect, but it occurs in a small percentage of patients. Most individuals tolerate statins well, and for those who experience muscle symptoms, discontinuing the medication typically resolves the issue.
Myopathy, while a recognized potential side effect of statin medications, is a relatively rare occurrence, affecting only a small percentage of patients. The vast majority of individuals who embark on statin therapy do so without experiencing any significant issues, and for those who do encounter muscle-related symptoms, there’s often a silver lining in the form of manageable solutions.
It’s important to emphasize that statins are generally well-tolerated by a wide range of patients. These medications have been a cornerstone in cholesterol management, and their benefits in reducing the risk of heart disease and stroke far outweigh the risks associated with myopathy.
For those who do encounter muscle-related symptoms while on statins, it’s reassuring to know that discontinuing the medication often leads to a resolution of the issue. Muscle symptoms can include pain, tenderness, or weakness, and they typically subside once the statin is stopped. In some cases, a healthcare provider may recommend a different statin or a lower dose if the cholesterol-lowering benefits are deemed essential for the patient.
Moreover, ongoing research is shedding light on the factors that can contribute to myopathy, allowing healthcare providers to better identify individuals at higher risk. This research-driven approach enables more precise prescribing and monitoring, further minimizing the chances of encountering this side effect.
In conclusion, while myopathy is a potential concern associated with statins, it’s important to keep it in perspective. The occurrence is rare, and for most individuals, statin therapy proceeds smoothly, providing substantial cardiovascular benefits. In cases where muscle-related symptoms do arise, discontinuing the medication is often sufficient to address the issue. With careful monitoring, tailored treatment plans, and ongoing research, statin therapy remains a valuable tool in the pursuit of heart health.
For a comprehensive look at this subject, we invite you to read more on this dedicated page: 3 Myths About Cholesterol-Lowering Statin Drugs | Johns Hopkins …
The evidence on statins causing cognitive impairment is inconclusive. While some studies suggest a link, the majority show no significant impact on cognitive function. The potential benefits in reducing cardiovascular risk often outweigh any perceived risks.
The evidence on statins causing cognitive impairment remains inconclusive, and the topic has generated significant debate among researchers and healthcare professionals. While some studies have suggested a potential link between statin use and cognitive issues, it’s crucial to consider the broader context:
Mixed Findings: Research on this topic has produced mixed findings. While a minority of studies have reported instances of cognitive impairment associated with statin use, the majority have found no significant impact on cognitive function. This inconsistency underscores the complexity of the issue.
Individual Variation: Responses to medications, including statins, can vary widely among individuals. Some people may experience side effects, including cognitive changes, while others may not. It’s essential for healthcare providers to consider these variations when prescribing statins.
Potential Benefits: Statins have consistently demonstrated their effectiveness in reducing LDL (bad) cholesterol levels and lowering the risk of cardiovascular events, such as heart attacks and strokes. These benefits can be especially significant for individuals with a history of cardiovascular disease or high cholesterol levels.
Shared Decision-Making: The decision to use statins should be a collaborative one between the patient and their healthcare provider. It should take into account the individual’s cardiovascular risk, medical history, and concerns about potential side effects, including cognitive effects.
Regular Monitoring: For those on statin therapy, regular monitoring of cognitive function is advisable, particularly if they have concerns or are at higher risk due to age or other factors. Any perceived cognitive changes should be discussed promptly with a healthcare provider.
Lifestyle Factors: Lifestyle factors such as diet, exercise, and overall cardiovascular health play a crucial role in cognitive function. Addressing these factors alongside statin therapy can contribute to better overall health and cognitive well-being.
Ongoing Research: The scientific community continues to study the potential relationship between statins and cognitive function. Ongoing research aims to provide more clarity on this complex issue, potentially shedding light on who may be more susceptible to cognitive effects, if any.
In summary, while concerns about statins and cognitive impairment exist, the evidence remains inconclusive. It’s essential to approach this topic with a balanced perspective, recognizing the potential benefits of statins in reducing cardiovascular risk, especially for individuals at high risk. Healthcare providers should engage in open communication with patients, considering individual factors, and monitor cognitive function when appropriate. Ultimately, the decision to use statins should be based on a thorough assessment of both the potential benefits and any perceived risks.
You can also read more about this here: 3 Top Statin Myths Debunked
Addressing the concern of overprescribing statins involves a careful assessment of an individual’s cardiovascular risk. Guidelines recommend statin therapy for those at high risk, such as individuals with a history of heart disease or diabetes.
Addressing the concern of overprescribing statins is a crucial aspect of responsible healthcare, as unnecessary medication use can lead to potential side effects and increased healthcare costs. To strike the right balance in prescribing statins, healthcare providers must conduct a thorough assessment of an individual’s cardiovascular risk.
Guidelines play a pivotal role in this assessment. They provide evidence-based recommendations that help healthcare providers identify individuals who stand to benefit the most from statin therapy. While these guidelines typically emphasize high-risk groups, such as those with a history of heart disease or diabetes, they also consider other factors that contribute to an individual’s overall cardiovascular risk.
One such factor is age. Older adults often face an elevated risk of heart disease, and guidelines may recommend statin therapy for those within a certain age range, particularly if they have additional risk factors. On the other hand, younger individuals with fewer risk factors may not require statins.
Cholesterol levels are another essential consideration. If an individual’s LDL (low-density lipoprotein) cholesterol is significantly elevated, even in the absence of other risk factors, it may warrant statin therapy. However, healthcare providers should also consider the entire lipid profile, taking into account HDL (high-density lipoprotein) cholesterol and triglyceride levels.
Family history of heart disease is yet another significant factor. If close relatives have experienced cardiovascular events at a relatively young age, this may elevate an individual’s risk and influence the decision to prescribe statins.
Smoking, high blood pressure, and obesity are additional risk factors that healthcare providers consider when assessing a patient’s cardiovascular risk. These lifestyle-related factors, when present, can further emphasize the importance of statin therapy in managing and reducing the risk of heart disease.
Ultimately, the decision to prescribe statins should involve a shared discussion between the healthcare provider and the patient. It’s important for individuals to be well-informed about their cardiovascular risk factors and the potential benefits and risks of statin therapy. This collaborative approach allows patients to actively participate in decisions about their healthcare and ensures that treatments are tailored to their unique circumstances.
By carefully assessing cardiovascular risk and adhering to evidence-based guidelines, healthcare providers can strike the right balance, ensuring that statin therapy is prescribed appropriately to those who will derive the most benefit while avoiding unnecessary medication use in low-risk individuals.
Looking for more insights? You’ll find them right here in our extended coverage: One cardiologist’s mission to reduce statin use for cholesterol | CNN

The affordability and accessibility of statins can be a concern. However, the availability of generic versions has made these medications more affordable, increasing access for many patients.
The affordability and accessibility of medications are crucial factors in ensuring that people receive the healthcare they need. Statins, being a vital component in managing cholesterol levels and preventing cardiovascular events, have faced concerns regarding their cost and availability. However, there have been significant developments that have improved the situation.
One of the most noteworthy developments is the availability of generic versions of statins. When a brand-name medication’s patent expires, it allows other pharmaceutical companies to produce and market generic versions of the drug. Generic statins are essentially the same as their brand-name counterparts in terms of active ingredients, safety, and effectiveness. The key difference lies in the price.
The introduction of generic statins has substantially reduced the cost of these medications. This reduction has made them more affordable for a broader range of patients, improving access to a critical component of cardiovascular care. Many healthcare systems and insurance plans now prefer to cover generic versions of statins as a cost-effective means of managing cholesterol levels.
Increased affordability and accessibility of statins have had a positive impact on public health. More individuals at risk of heart disease can now afford and access these medications, potentially preventing heart attacks and strokes. This is particularly important for individuals with limited financial means who may have previously struggled to afford essential medications.
Moreover, healthcare providers have a role to play in addressing cost concerns. They can work with patients to explore available options, including generic statins and patient assistance programs, to ensure that financial considerations do not hinder the appropriate management of cholesterol and cardiovascular risk.
However, it’s essential to remember that medication affordability remains a complex issue. In some cases, patients may still face barriers to access due to factors like insurance coverage, regional variations in drug pricing, or healthcare disparities. Continual efforts are necessary to address these challenges and make sure that everyone who can benefit from statin therapy can access it without undue financial burden.
In summary, the availability of generic statins has significantly improved the affordability and accessibility of these critical medications. This development has widened the scope of individuals who can benefit from cholesterol management, ultimately contributing to better cardiovascular health outcomes. Still, there is work to be done to ensure that healthcare systems and policies support equitable access to essential medications for all patients.
Don’t stop here; you can continue your exploration by following this link for more details: Flawed cholesterol study makes headlines – Heart Matters magazine …

The controversies surrounding statin use emphasize the importance of informed decision-making. It’s crucial for individuals to work closely with their healthcare providers to assess their unique cardiovascular risk and determine the most appropriate treatment plan. While statins may not be suitable for everyone, they remain a valuable tool in managing cholesterol and reducing cardiovascular risk for many individuals.
Ultimately, the benefits of statin therapy in preventing heart disease and strokes are well-established. Debunking myths and addressing concerns with evidence-based information can help individuals make informed choices about their cardiovascular health, leading to better outcomes and improved overall well-being.
Looking for more insights? You’ll find them right here in our extended coverage: Some Myths about Nutrition & Physical Activity – NIDDK
More links
Explore this link for a more extensive examination of the topic: 3 Myths About Cholesterol-Lowering Statin Drugs | Johns Hopkins …
